I spent years trying to conceive through IVF – 40 years after Louise Brown, it’s time we were honest about the treatment
Even with the new add-ons and decades of scientific advances, success rates for women under 35 are relatively low, and private treatment remains unaffordable
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
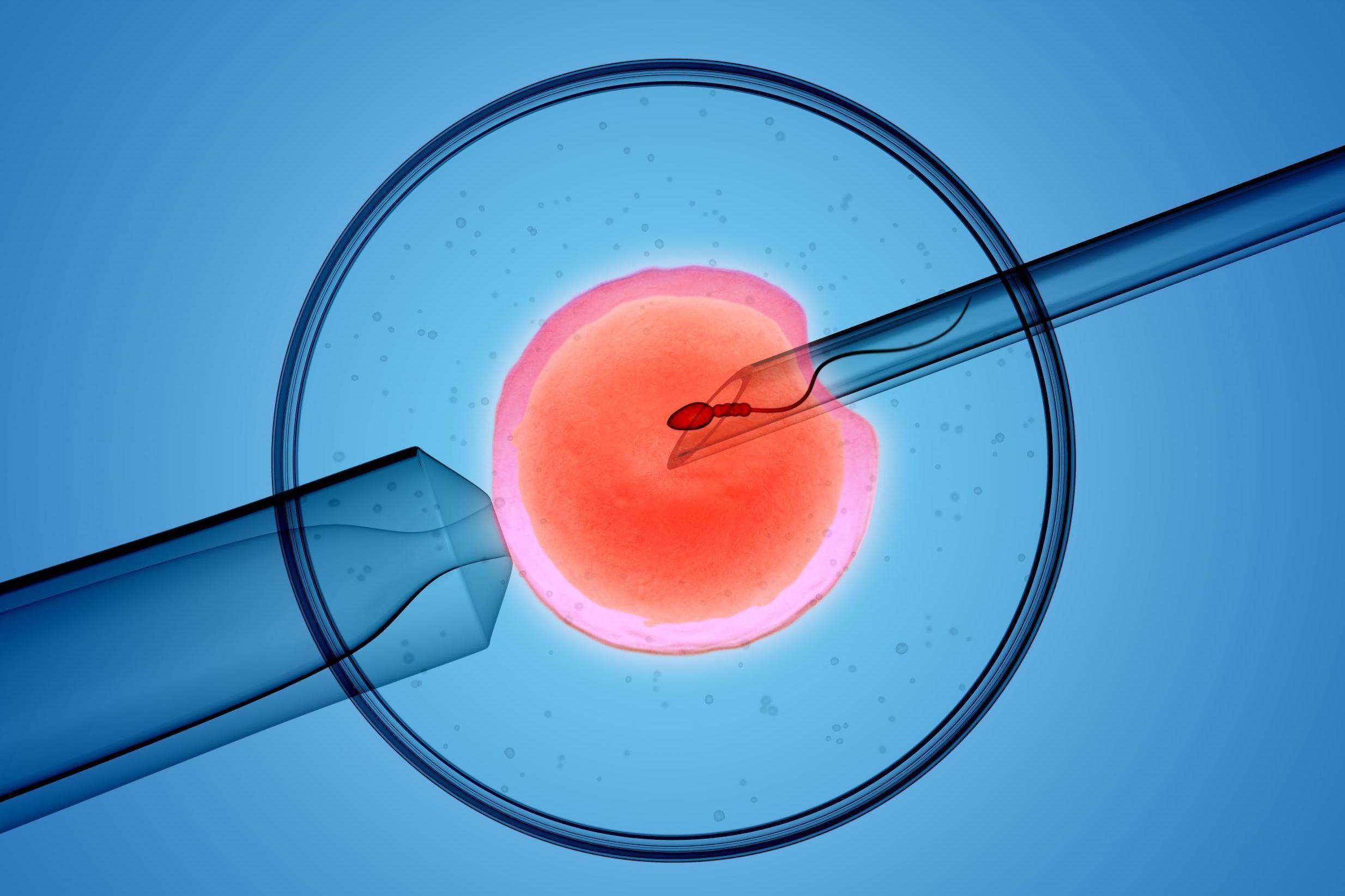
Your support makes all the difference.You would have to be on a different planet to have missed the news that this week the world’s first “Test Tube Baby”, Louise Brown, turns 40. It means IVF has reached its own birthday milestone, bringing to childless couples its own unique layering of joy and disappointment.
My own experience of IVF is somewhat “vintage”. My husband and I went through five cycles of unsuccessful IVF in the 1990s when IVF was a fresh-faced and evolving medical technique. But even back when we had our treatment, IVF was hugely expensive.
We had no access to NHS funding and this was not down to where we lived or my age; it was because my husband had children from his previous marriage. “Failing” this one criterion left me feeling completely bereft. I felt that as an individual without children I deserved to be supported by the system I had paid into all my working life. Counting all our consultations, medication and treatments, we spent over £30,000. Our final cycle was funded by a home improvement loan (technically, a child would have improved our home).
The National Institute for Clinical Excellence recommends that three cycles of IVF be offered as standard. But in England, just 12 per cent of clinical commissioning groups (CCGs) offer this gold standard. It shouldn’t be a lottery. Infertility is a medical condition that causes despair, destroys relationships and changes lives forever. Treatment should be offered according to universal and fair criteria. We shouldn’t have to consider packing up and moving to another county – or even another country – to access treatment.
We were lucky. We could just about afford our five cycles of IVF. But it makes me wonder about all those that do not quite match the criteria, or who live in the wrong postcode and who are too financially stretched to undergo private treatment.
When we had our treatment, things were relatively uncomplicated – you were offered one or two treatment techniques. Now there is a plethora of supplementary treatments offered, at extra cost, at most fertility clinics. The Human Fertilisation and Embryology Authority (HFEA) website lists nine of these “add-ons” all with varying degrees of evidence-based research to back them up.
In my work as a fertility counsellor, I have listened to clients agonise over whether to spend yet more of their precious savings – or their family’s savings – on an extra treatment that may or may not increase their chances of conceiving. Being faced with such decisions at a time when you are incredibly vulnerable is a challenging prospect.
During our final treatment, “assisted hatching” was mentioned as a new technique we could consider for subsequent cycles. Sadly, that cycle ended in miscarriage and we had come to the end of the line physically, psychologically and financially. Looking now at the HFEA’s assessment of the efficacy of assisted hatching, I’m so pleased we were spared the turmoil of having to decide whether or not to buy into something that offered us a little more hope without much more certainty.
There is a growing swell of opinion now that more regulation is needed for these add-ons. I believe that, at the very least, clinics should be pressed to be completely transparent about the potential clinical outcomes of these supplementary treatments and to offer clearly described details of research and any clinical studies that have been carried out.
Worldwide, possibly eight million children exist today because of IVF. Nevertheless, even with the new add-ons and 40 years of scientific advances, IVF is still not a panacea. Success rates for women under 35 are still only 29 per cent in the UK. That means about two-thirds of fertility patients will emerge from treatment without the miracle they so wished for. Despite these statistics, thousands of us will buy, body, soul and wallet, into the hope that IVF offers, believing – as we did – that they will be one of the lucky third.
Deborah Sloan is a writer and therapist. She blogs about childlessness at Without Issue
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments