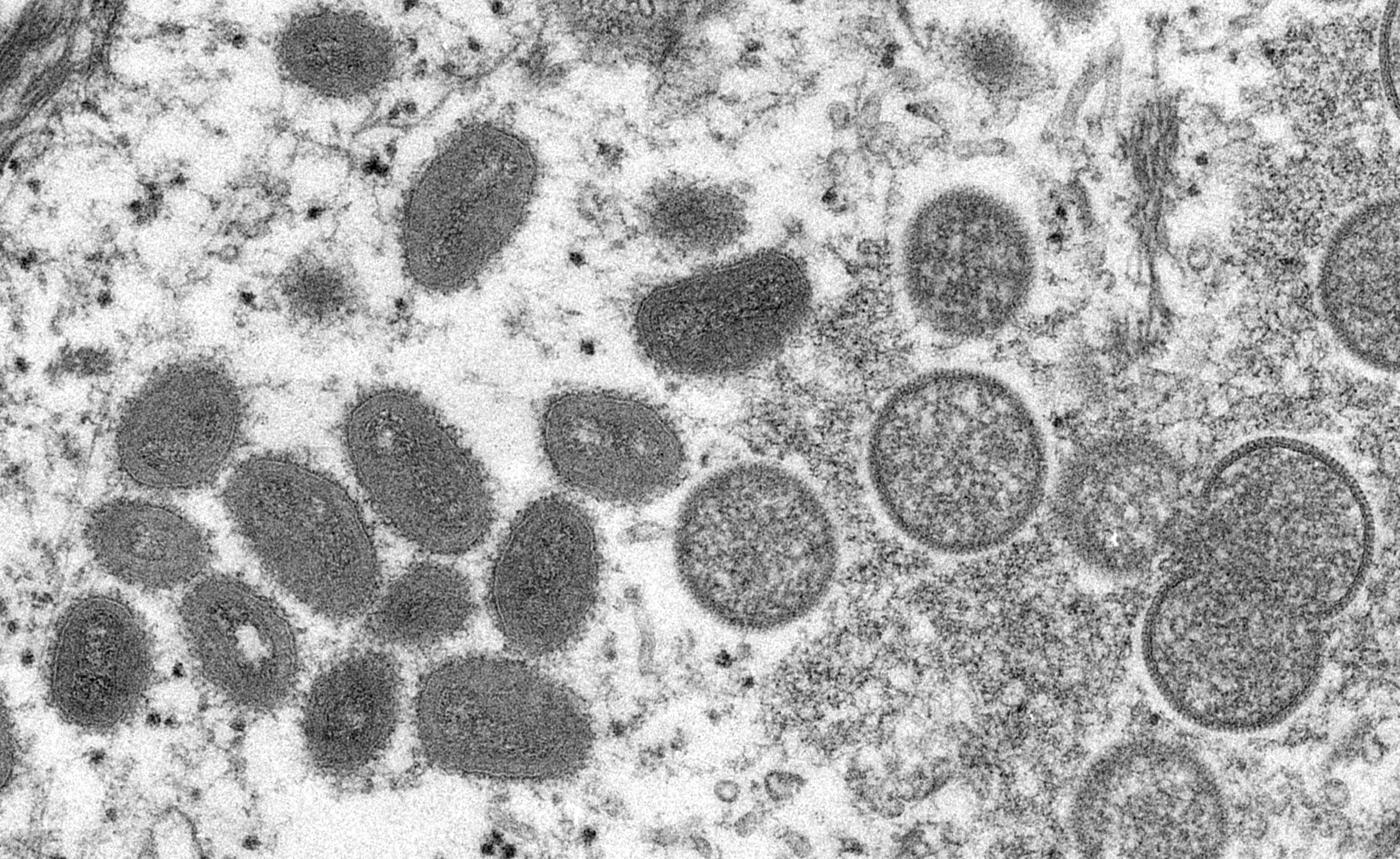
Monkeypox: Confirmed cases in the UK rise to 78
Further seven infections detected in England
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.The number of confirmed cases of monkeypox in the UK has risen to 78, after a further seven infections were identified in England.
Despite further cases being detected, the risk to the general population remains low, the UK Health Security Agency (UKHSA) said – though scientists are concerned at the prospect of the virus spreading in animals and pets, which could become a permanent reservoir for the viral infection.
To date, no cases have been identified in Wales and Northern Ireland. One infection has been detected in Scotland, while 77 have now been reported across England since 7 May.
UKHSA said a notable proportion of the cases identified to date have been among people who are gay and bisexual, adding that these groups should be alert to new rashes or lesions that form on any part of their body.
Dr Susan Hopkins, chief medical adviser at UKHSA, said: “We are continuing to promptly identify further monkeypox cases in England through our extensive surveillance and contact tracing networks, our vigilant NHS services, and thanks to people coming forward with symptoms.”
Those who suspect they may have symptoms have been encouraged to limit their contact with others and ring 111 or visit their local sexual health service “as soon as possible”.
People who come into contact with infected individuals are being offered a vaccine typically used to protect against smallpox, which is caused by a similar virus.
This strategy, known as ring vaccination, includes health care workers, sexual partners and housemates. High-risk contacts are also being asked to isolate at home for three weeks, as the virus has a long incubation time and it can take several weeks for symptoms to emerge.
Nearly 20 countries where monkeypox is not endemic have reported outbreaks of the disease, with more than 130 confirmed or suspected infections detected, mostly in Europe.
The World Health Organisation has described the sudden increase in cases as “atypical”, but said the outbreak remains “containable” and limited. The fact that cases are being seen in so many different countries suggests the infection may have been silently spreading for some time, the agency said.
Monkeypox is usually found in west Africa, and the virus does not tend to spread easily between people. The illness is usually mild and those who are infected with the virus typically recover in a matter of weeks.
Symptoms include fever, headache, muscle aches, backache, swollen lymph nodes, chills and exhaustion. A rash can develop, often beginning on the face, which then spreads to other parts of the body including the genitals.
The first case identified in the UK was in a person who had returned from Nigeria, but other cases are unrelated to travel.
Sir Jeremy Farrar, the director of the Wellcome Trust, said “we have never seen anything like this before, with such a number of cases” in so many countries.
Speaking on Monday, he told BBC Radio 4’s Today programme that there have been small outbreaks in the past, with cases recorded in the UK, but “this is different, something has changed” and suggested superspreader events could be responsible.
“The virus may have changed, but I think that's unlikely,” Sir Jeremy said. “More likely is, I think, that the niche that this virus now finds itself in has allowed for some superspreader events and those individuals involved in that have then travelled to other parts of the world and taken the infection with them.”
A leading adviser to the WHO similarly described the outbreak of cases as “a random event” that might be explained by two recent mass events in Europe.
Dr David Heymann, who formerly headed WHO’s emergencies department, said the leading theory to explain the spread of the disease was sexual transmission – and the close contact that it brings.
“We know monkeypox can spread when there is close contact with the lesions of someone who is infected, and it looks like sexual contact has now amplified that transmission,” said Dr Heymann.
That marks a significant departure from the disease’s typical pattern of spread in central and western Africa, where people are mainly infected by animals, such as wild rodents and primates, and outbreaks have not spread across borders.
The disease can be fatal in up to 10 per cent of infections, but no deaths have been reported among the current cases.
As health officials race to understand and contain the ongoing outbreak, the European Centre for Disease Control warned that it was important to “manage exposed pets and prevent the disease from being transmitted to wildlife”.
“If human-to-animal transmission occurs, and the virus spreads in an animal population, there is a risk that the disease could become endemic in Europe,” the agency said.
Scientists have pointed out that it will be difficult to disentangle whether it is sex itself or the close contact related to sex that has driven the recent spread of monkeypox across Europe.
“By nature, sexual activity involves intimate contact, which one would expect to increase the likelihood of transmission, whatever a person’s sexual orientation and irrespective of the mode of transmission,” said Mike Skinner, a virologist at Imperial College London.



Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments