The Independent's journalism is supported by our readers. When you purchase through links on our site, we may earn commission.
Why the latest cancer treatment breakthrough could change everything
A newly discovered method seems to hold the key to being able to target every cell in a tumour
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Over the past few years, immunotherapies – treatments which harness the power of the immune system to fight cancer – have been making headlines around the world. But the biggest challenges for immunotherapy have been identifying which molecules on the cancer cells are the best targets, as well as how to get past cancer’s defences.
For now, the immunotherapy treatments available to patients are powerful but blunt weapons, which in some cases can result in a number of potentially serious side effects. What is urgently needed are treatments that can guide immune cells to specifically attack a tumour, while leaving healthy cells alone. And it may have just been discovered. Cancer Research UK scientists have published a new study that has potentially uncovered the intelligence needed to precisely guide these new weapons.
Scientists have tried many different approaches to turn the immune system against cancer, such as cutting the brakes on immune cells, flagging certain cells for destruction, or genetically engineering a patient’s immune cells to directly target cancer cells.
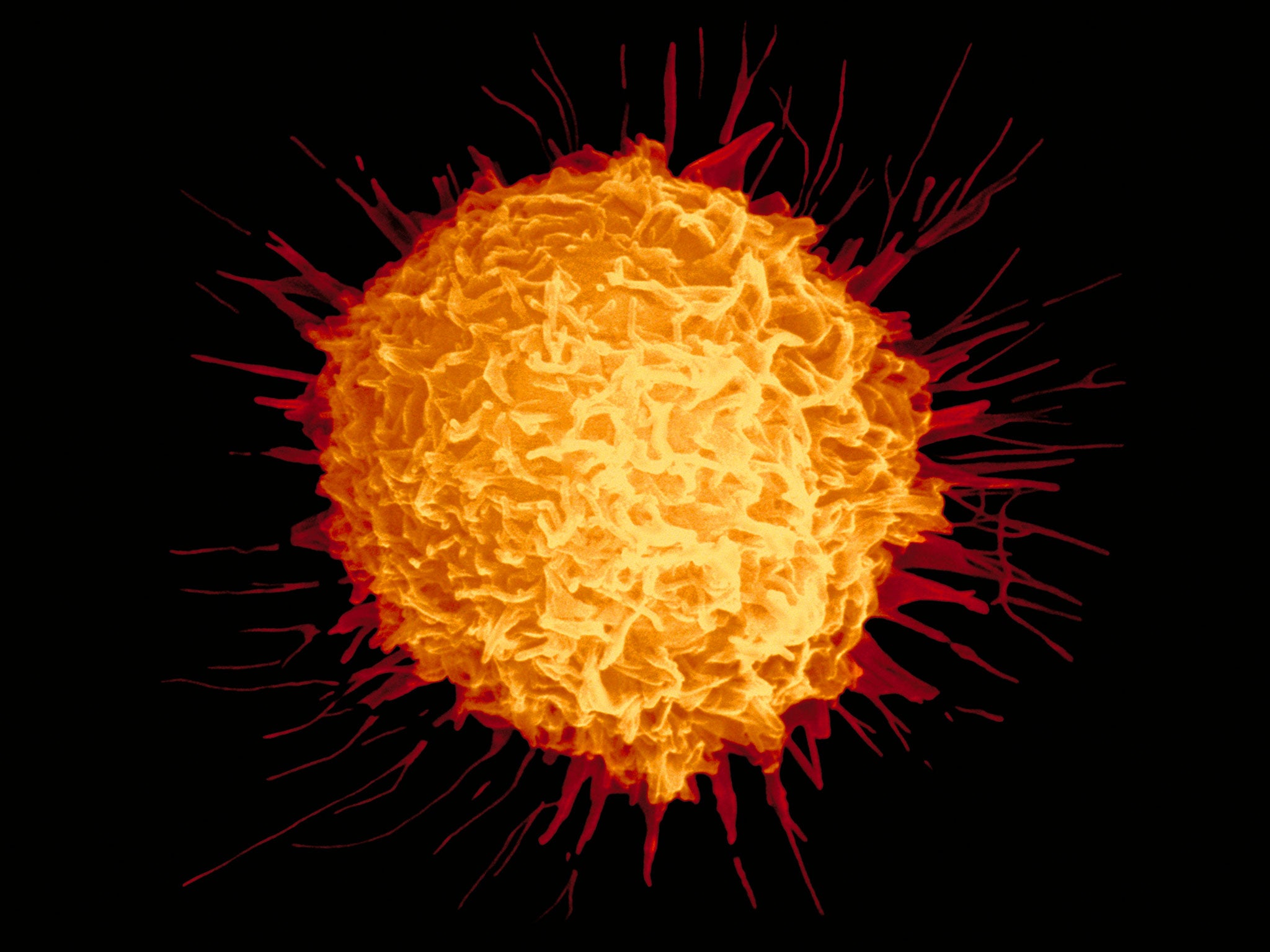
But most of these depend on the immune system being able to recognise cancer cells as the true threat that they are. To do this, specialised immune cells – called T-cells – have to spot the danger signals, or "flags" on the surface of cancer cells.
Once the immune system recognises a cancer specific "flag" it should destroy all cancer cells that carry it. But this doesn’t always happen. So developing better immunotherapies relies on figuring out which “flags” make the best targets for the immune system to attack. And we now have a way of doing that.
Tumours change as they grow, building up more and more changes in their genetic code. And it turns out that this overwhelming genetic complexity, which can make cancers so resistant to certain treatments, may actually make them visible to the immune system.
Today’s discovery builds on the idea that some early DNA faults in a tumour’s evolutionary history can persist all the way through its development. And the researchers have shown that some of these early events are being presented as “flags” on the surface of all tumour cells, where they provide an ideal target for the immune system to attack.
Crucially, they have turned this discovery into a computer prediction method to spot the flags that are shared across all tumour cells, based on genetic tumour data.
Using this method they were able to "fish out" immune cells from two lung tumour samples that recognised and latched on to the shared flags.
The hope is that this method could be developed into a way of fishing out the best immune T-cells that target every cell in a tumour. If these immune cells could be isolated and multiplied in the lab, they may offer a potent treatment alongside current therapies that release the “brakes” on the immune system.
Or, the “flags” themselves may even be enough to awaken the immune system, which is why many believe this could be a step towards personalised vaccines to target an individual patient’s tumour.
For the first time, this study shows that there are “good” and “bad” targets for immunotherapy treatments. And it gives us a way of predicting what the good targets will be.
It’s early days, but teams are now working to turn this idea into something that could be applied to many more cancers, finding unique targets on all cancer cells and not just the healthy ones.
And, most importantly, this may provide the tools necessary to give immunotherapy the precision guidance that will make a difference for patients in the future.
Professor Peter Johnson is chief clinician at Cancer Research UK
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments