Monkeypox and travel: Everything you need to know
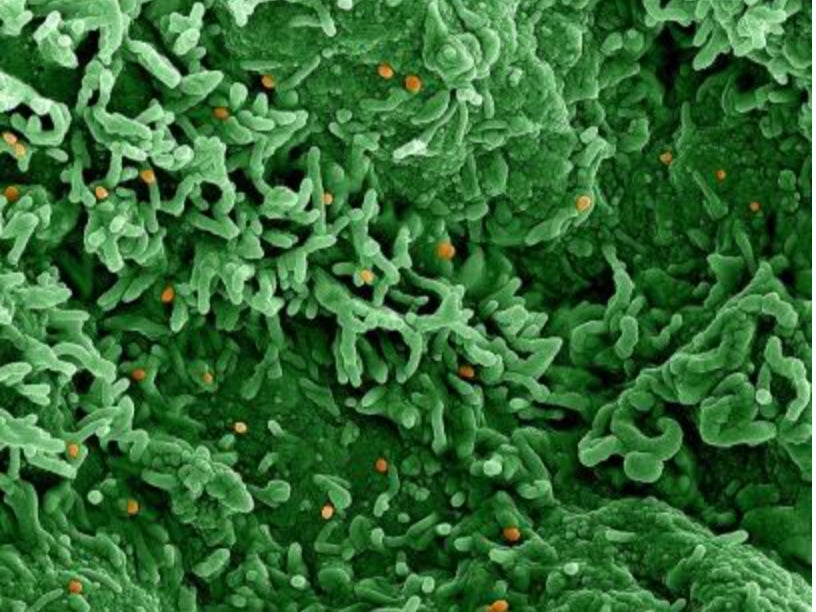
‘The first human case of monkeypox was recorded in 1970 in the Democratic Republic of the Congo’ – US National Institute of Allergy and Infectious Diseases
The World Health Organisation (WHO) has declared monkeypox a global health emergency and issued some travel recommendations for people who may be infected.
These are the key questions and answers.
What is monkeypox?
A rare infection most commonly found in west and central Africa, but currently spreading worldwide – with an estimated 16,000 cases. It was first discovered among colonies of monkeys in 1958.
“The first human case of monkeypox was recorded in 1970 in the Democratic Republic of the Congo,” says the US National Institute of Allergy and Infectious Diseases.
“The disease is endemic in central and western Africa, and infections linked to international travel or imported animals have occurred in Israel, Singapore, the United Kingdom, and the United States.”
The NHS says: “Monkeypox is usually mild and most people recover within a few weeks without treatment.
“But, if your symptoms are more severe and you become unwell, you may need treatment in hospital.”
The first symptoms of monkeypox usually appear between five days and three weeks after infection. They include:
- high temperature
- headache
- muscle aches
- backache
- swollen glands
- shivering (chills)
- exhaustion
Between one and five days after the initial symptoms, a rash usually appears – often on the face, then spreading to other parts of the body, including the genitals and anus.
The NHS says: “The rash is sometimes confused with chickenpox. It starts as raised spots, which turn into small blisters filled with fluid.
“These blisters eventually form scabs which later fall off.”
Could I end up in hospital?
“Monkeypox is usually mild,” says the NHS. “Most people recover within a few weeks without treatment.
“But, if your symptoms are more severe and you become unwell, you may need treatment in hospital.”
The likelihood of needing treatment in hospital is highest for:
- older people
- young children
- people with a condition or who are taking a medicine that affects their immune system
Symptoms usually clear up within a few weeks. While carriers are symptomatic, they can pass monkeypox on to other people.
How can I avoid catching monkeypox?
The NHS recommends the following:
- wash your hands with soap and water regularly or use an alcohol-based hand sanitiser
- talk to sexual partners about their sexual health and any symptoms they may have
- be aware of the symptoms of monkeypox if you are sexually active, especially if you have new sexual partners
- take a break from sex and intimate contact if you have symptoms of monkeypox until you get seen by a doctor and told you are no longer at risk of passing it on
- do not share bedding or towels with people who may have monkeypox
- do not have close contact (within 1 metre) with people who may have monkeypox
- do not go near wild or stray animals, including animals that appear unwell or are dead, while travelling in west and central Africa
- do not eat or touch meat from wild animals while travelling in west and central Africa
What travel rules are there – and who do they affect?
The World Health Organisation says three categories of people should avoid travel, including international journeys:
- those with signs and symptoms compatible with monkeypox virus infection
- those considered a “suspect, probable, or confirmed case of monkeypox by jurisdictional health authorities”
- those who have been identified as contacts of a monkeypox case and, therefore, is subject to health monitoring.
“Exemptions include any individual who need to undertake travel to seek urgent medical care or flee from life-threatening situations, such as conflict or natural disasters,” says the WHO.
MPs on the Public Accounts Committee say: “In the longer term, health measures may be needed to deal with new variants of Covid-19 or other diseases such as monkeypox.”
Is there a vaccine?
Monkeypox is caused by a virus that is similar to smallpox – though much less harmful. The smallpox vaccine (known as MVA) is believed to give a good level of protection against monkeypox. The NHS is offering a single dose of MVA to people who are most likely to be exposed to monkeypox, in order “to help reduce the severity of monkeypox symptoms and prevent future infections”. Those at most risk are:
- some healthcare workers
- some men who are gay, bisexual or have sex with other men
- people who have been in close contact with someone who has monkeypox
The NHS says those at risk of exposure will be contacted and offer you a vaccine. Check the website of your local sexual health service for more information.
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies