Transplant hope for minorities as researchers alter donor kidney blood type
The development could increase the supply of kidneys available for transplant.
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Researchers have successfully altered the blood type of three donor kidneys in a game-changing discovery that could have a massive impact on patients waiting for a transplant.
The development could increase the supply of kidneys available for transplant, particularly within ethnic minority groups who are less likely to find a match, scientists say.
A kidney from someone with an A blood type cannot be transplanted to someone with a B blood type, nor the other way around.
The research that Mike and Serena are undertaking is potentially game-changing
But changing the blood type to the universal O will allow more transplants to take place as this can be used for people with any blood type.
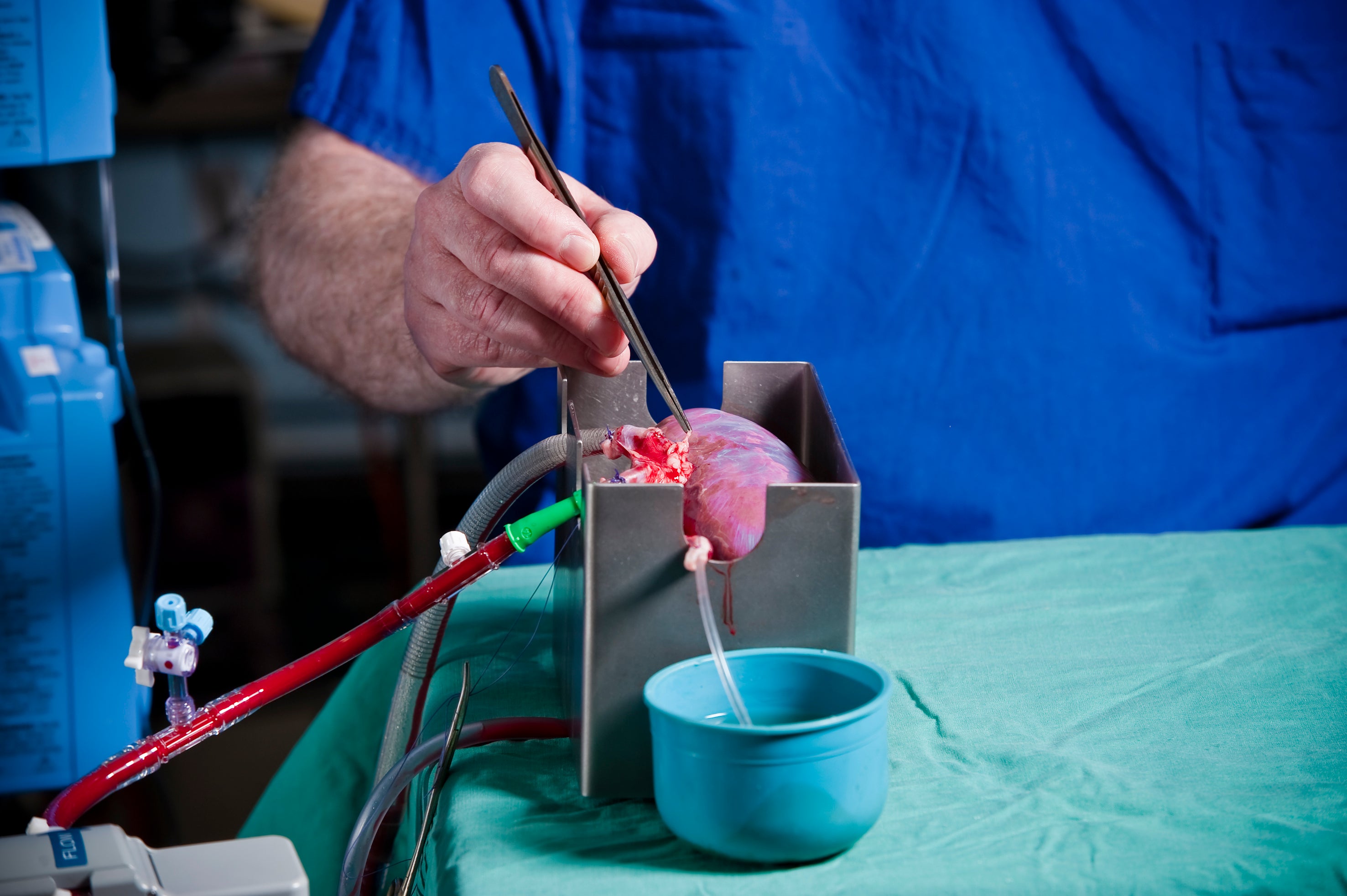
University of Cambridge researchers used a normothermic perfusion machine – a device which connects with a human kidney to pass oxygenated blood through the organ to better preserve it for future use – to flush blood infused with an enzyme through the deceased donor kidney.
The enzyme removed the blood type markers that line the blood vessels of the kidney, which led to the organ being converted to O type.
Serena MacMillan PhD student at the University of Cambridge said: “Our confidence was really boosted after we applied the enzyme to a piece of human kidney tissue and saw very quickly that the antigens were removed.
“After this, we knew that the process is feasible, and we just had to scale up the project to apply the enzyme to full-size human kidneys.
“By taking B type human kidneys and pumping the enzyme through the organ using our normothermic perfusion machine, we saw in a matter of just a few hours that we had converted a B type kidney into an O type.
“It’s very exciting to think about how this could potentially impact so many lives.”
People from ethnic minority groups often wait a year longer for a transplant than white patients, and so the study could have particular implications for them, experts say.
People from minority communities are more likely to have B type blood and with current low donation rates from these populations, there are not enough kidneys to go around.
In 2020/21, just over 9% of total organ donations came from black and minority ethnic donors while black and minority ethnic patients make up 33% of the kidney transplant waiting list.
Now the researchers need to see how the newly changed O type kidney will react to a patient’s usual blood type in their normal blood supply.
The machine allows them to do this before testing in people, as they can take the kidneys which have been changed to the O type, and introduce different blood types to monitor how the kidney might react.
Professor Mike Nicholson, professor of transplant surgery at the University of Cambridge said: “One of the biggest restrictions to who a donated kidney can be transplanted to is the fact that you have to be blood group compatible.
“The reason for this is that you have antigens and markers on your cells that can be either A or B.
“Your body naturally produces antibodies against the ones you don’t have.
“Blood group classification is also determined via ethnicity and ethnic minority groups are more likely to have the rarer B type. ”
Dr Aisling McMahon, executive director of research at Kidney Research UK said: “The research that Mike and Serena are undertaking is potentially game-changing.”
After testing the reintroduction of other blood types, the team will look at how the approach might be used in a clinical setting.
The research, which is funded by charity Kidney Research UK, is due to be published in the British Journal of Surgery in the coming months.
Ayesha, from Bury in Greater Manchester, was diagnosed with stage three chronic kidney disease in 1998 when she was pregnant with her first child.
Her kidneys deteriorated rapidly during the pandemic and she was told that she would need a transplant, but she might have to wait double or even triple the time for a kidney than a white person.
The research will offer so much hope to minority groups still waiting for a transplant and could help to save many lives
Consultants estimated she might have to wait between six to 10 years to receive one.
Ayesha said: “They explained that because of my ethnicity my wait for a deceased donor will be longer than for a white person.
“The reason being my background – being the Muslim community and other faiths and cultures often don’t agree to be organ donors.
“I feel sad at the thought of waiting so long for a transplant. I understand a transplant isn’t a cure, but it would make my body a lot stronger and give me a second chance at a healthy life.”
She added: “Even after the law change so everyone was automatically made an organ donor, many people decided to opt out.
“The research will offer so much hope to minority groups still waiting for a transplant and could help to save many lives.
“Convincing communities that research such as this and organ donation is beneficial is so crucial to improving and saving lives.”