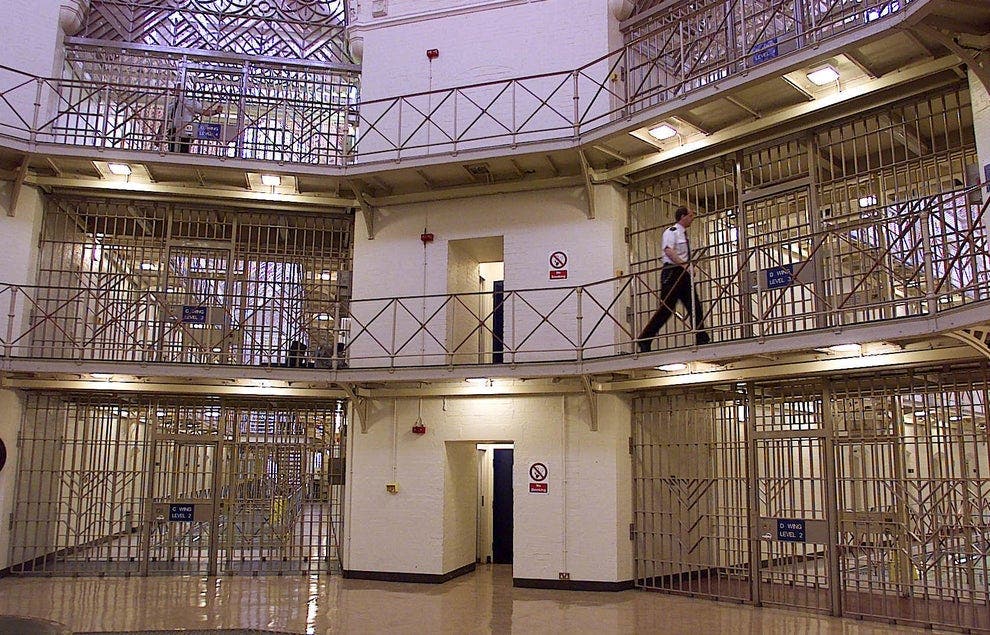
Prisoners three times more likely to miss hospital appointments with no notice than general public, says report
‘Worrying signs’ Covid-19 measures have ‘worsened’ poor access to healthcare in jails, says Nuffield Trust
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Prisoners are three times as likely to miss hospital appointments with no advance notice than the general population, according to new findings.
Research by the Nuffield Trust find that the pandemic, on top of existing prison staff shortages and overcrowding, may have worsened already poor access to healthcare in jails.
The report, seen by The Independent, finds that in 2019/20, prisoners missed 42 per cent of scheduled outpatient appointments, compared with 23 per cent in the community.
The percentage of missed appointments where no advanced warning was given was 18 per cent - three times higher than in the general population (6 per cent).
Researchers warn that missed appointments risk making health conditions worse for prisoners when they are finally seen - which is particularly concerning given that many enter prison with specific health needs related to their mental health or alcohol and drug-related disorders.
Although the research covers only the first month of the pandemic, the hospital data shows that in March 2020 there was a 16 per cent drop in emergency admissions compared with the previous month.
Admissions to hospital were also reduced in the general public, but researchers said the considerable drop seen in jails was concerning given the extended lockdowns in prisons and staff shortages which have remained throughout the pandemic.
The report notes that prison escort availability remains a “key cause” of missed appointments. At a time when the prison estate is more overcrowded than ever and the populations continues to grow, there are 12 per cent fewer staff working in prisons now than in 2010.
Report author and Nuffield Trust senior fellow Dr Miranda Davies acknowledged that the full impact of the pandemic hasn’t yet been seen, but said: "There are worrying signs that the measures put in place to protect prison staff and prisoners from Covid-19 are actually worsening the poor access to essential hospital care that prisoners already faced.
"We know that even before the pandemic, the prison estate was holding more prisoners than it was ever designed for. On top of this, the loss of experienced prison staff means conditions in prisons are challenging and prisoners just aren’t getting the access to health services they need.”
A Prison Service spokesperson said it would consider the findings of the report with health partners, adding: “Our decisive action saved thousands of lives during the pandemic.
“There is no evidence prison restrictions impacted access to healthcare. Lower rates of admissions were also mirrored in the community as non-critical appointments were cancelled due to the pandemic.”
The research, funded by the Health Foundation, also points to a lack of progress following warnings made in earlier research from February 2020, which revealed that missed or cancelled appointments in 2017/18 had cost the NHS £2m.
The previous report showed that 16 per cent of hospital appointments made for inmates were categorised as “did not attend – no advance warning given” – meaning the proportion has increased by 2 per cent in three years.
"Not only are more appointments being missed by those in prisons compared to the general public, our analysis also shows more needs to be done to understand the complex health risks, needs and challenges of those coming into prison,” Dr Davies added.
Peter Dawson, director of the Prison Reform Trust, said: “The government’s long established policy is that healthcare in prison should be neither better nor worse than it is in the community. This report shows that it is failing to deliver that policy on the ground.
“The government’s enthusiasm for putting ever more people in jail ignores its failure to provide even the most basic requirements of a decent and civilised penal system. Lives will be lost as a consequence.”
It comes after research by the University College London (UCL) last June found concerning practice around the treatment of prisoners when they are in hospitals, including being forced to wait in hospital cupboards before getting treatment and being required to undergo intimate medical examinations in the presence of prison guards.
Inmates reported having no prior knowledge or control over appointments, and experiencing significant delays in treatment due to cancellations and prison-to-prison transfers – potentially exacerbating their illness.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments