Landmark sickle cell disease inquiry finds evidence of racism in patient care
The findings form the basis of the most comprehensive report on sickle cell care in Whitehall’s history

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Sickle cell patients are grappling with racism in the NHS that is placing their lives at risk, a groundbreaking parliamentary report has highlighted.
The revelations have prompted cross-party MPs to urge health secretary Sajid Javid and the NHS to take urgent action in addressing this problem.
The findings have been set out in the No One’s Listening report, which was jointly published on Monday by the All-Party Parliamentary Group (APPG) on Sickle Cell and Thalassaemia and the Sickle Cell Society, a national charity that supports and represents people affected by sickle cell blood disorders.
Sickle cell predominantly affects black people, and patients shared with the APPG inquiry accounts of being treated with disrespect, not being believed or listened to, and having their pain disregarded and not treated as a priority by healthcare professionals, even in cases where urgent medical care was needed.
Some patients shared examples of particularly overt racism - one patient said he has “had to deal with doctors and nurses openly being racist towards me and others… I’ve been called the N-word to my face and much worse.”
“As sickle is mainly a black illness, they jump to the conclusion that we’re all ‘junkies’ and not in pain at all … If we were cancer patients it would be totally different, they have high doses of morphine, no questions asked and extra if they need it because they are mainly white people,” Diane Crawford, another patient, told the inquiry.
Led by the APPG chair Pat McFadden MP, the inquiry has been hailed as the most comprehensive report on sickle cell care that the parliamentary group, established in 2008, has ever published.
Mr McFadden said: “This report has shown us that whilst people living with sickle cell generally had high levels of confidence in specialist haematology departments, there was a big gulf between this and the experience of A&E departments and generalist wards.
“One of the key findings in the report was the lack of communication between these two areas when treating people with sickle cell; this, along with tragic and avoidable deaths, has caused a serious and damaging impact on the levels of trust in the health system among sickle cell patients.
“In preparing this report we took extensive oral and written evidence from sickle cell patients, clinicians and others. The report calls for a comprehensive transformation in the care of people living with sickle cell. It also reflects the frustration that many of these arguments have been made for a long time without a proper response.”
The Labour MP for Wolverhampton South East said he hopes that this report is “taken seriously” by the Department of Health and Social Care and by the NHS.
The inquiry also includes evidence of sub-standard care for sickle cell patients admitted to general wards or attending A&E departments, low awareness of sickle cell disease among healthcare professionals and examples of inadequate training and insufficient investment in sickle cell care.
In addition to these failings, there were frequent reports of negative attitudes towards sickle cell patients, and the inquiry found that these concerns have led to an avoidance of hospitals for many people living with sickle cell.
Earlier this year, The Independent reported that campaigners warned that sickle cell patients are being “ignored because they’re black”.

As part of its work, the APPG reviewed the case of sickle cell patient Evan Nathan Smith, 21, who died in North Middlesex University Hospital in April 2019 after calling 999 from his hospital bed while in crisis and being refused oxygen.
An inquest into his death in April 2021 found that he might still be alive were it not for failures in the care he received.
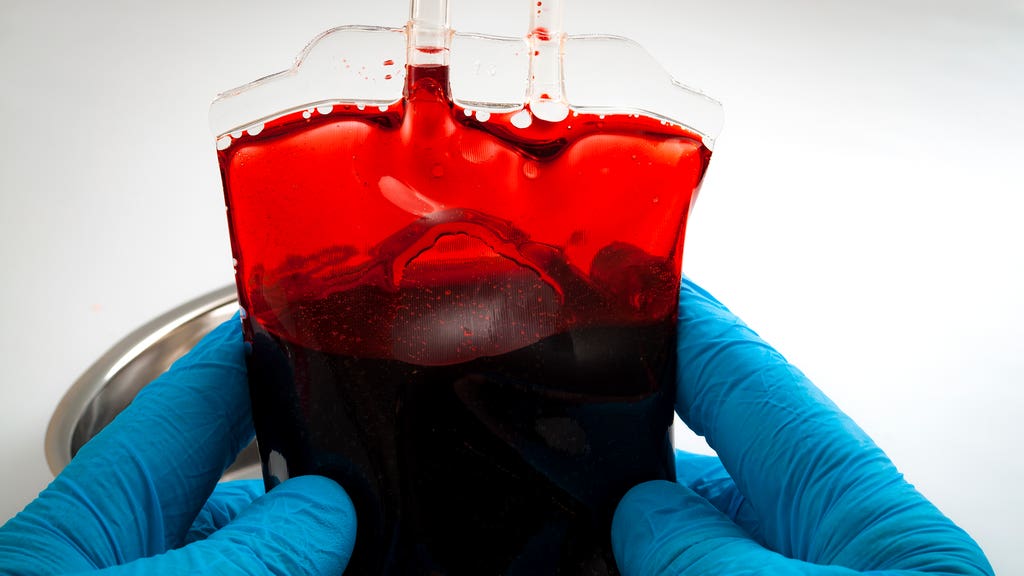
During what is known as a sickle cell crisis, blood vessels can become blocked by sickle cells, which starves muscles, organs and surrounding tissue of oxygen, causing severe pain that can last for days.
John James, CEO of the Sickle Cell Society, described this report as an “urgent call to action”, adding that it ought to be a turning point that addresses deep-seated failures of care.
“The APPG inquiry’s findings are appalling but will sadly not come as a surprise to many people who have found themselves in need of urgent medical help for the symptoms of sickle cell,” he said.
“The inquiry is the first of its kind as it featured oral evidence sessions with testimony from expert witnesses including sickle cell patients, patients’ carers and family members, clinicians and representatives from relevant healthcare bodies and over 100 submissions of written evidence from key stakeholders.”
It is estimated that there are between 12,500 and 15,000 people with sickle cell disease in the UK.
The illness forms a group of inherited blood conditions where people living with the condition produce unusually shaped red blood cells, which do not live as long as healthy cells and can block blood vessels.



Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments