The Independent's journalism is supported by our readers. When you purchase through links on our site, we may earn commission.
Scientists discover new type of cell hidden in human lungs that may lead to novel treatments
Respiratory airway secretory cells line tiny airway branches, deep in lungs, near alveoli air sacs where oxygen is exchanged for carbon dioxide
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Scientists have discovered a new type of cell hidden within human lungs which they say may play a key role in some respiratory diseases.
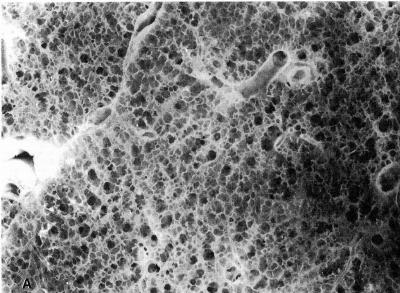
The study, published last week in the journal Nature, assessed human lung tissue samples and identified new cells called respiratory airway secretory cells (RASCs).
Researchers, including those from the University of Pennsylvania School of Medicine in the US, say these cells line tiny airway branches, deep in the lungs, near the alveoli air sacs where oxygen is exchanged for carbon dioxide.
RASCs, according to the study, have stem-cell-like properties that enable them to regenerate other cells that are essential for the normal functioning of alveoli.
Cigarette smoking and the common smoking-related ailment called chronic obstructive pulmonary disease (COPD) can disrupt the regenerative functions of RASCs, scientists say, adding that correcting this disruption may be a potential way to treat COPD.
People with COPD experience progressive damage to and loss of alveoli, which is exacerbated by chronic inflammation.
Reports suggest the condition causes about 3 million deaths every year around the world and affects nearly 10 per cent of people in some parts of the US.
While patients are mainly prescribed steroid drugs to reduce inflammation, along with oxygen therapy, scientists say these treatments can only slow the disease process and cannot stop or reverse it.
Earlier studies have found that another type of cells in the lungs called AT2 cells become abnormal in COPD and other lung diseases.
Researchers say scientific understanding of COPD has been gradual since mice, which are the standard lab animal models to study the condition, have lungs that lack key features of human lungs.
“COPD is a devastating and common disease, yet we really don’t understand the cellular biology of why or how some patients develop it. Identifying new cell types, in particular new progenitor cells, that are injured in COPD could really accelerate the development of new treatments,” study first author Maria Basil said in a statement.
In the new study, scientists uncovered evidence of the new types of cells RASCs while examining gene-activity signatures of lung cells sampled from healthy human donors.
They found that RASCs, which don’t exist in mice lungs, are “secretory” cells that reside near alveoli and produce proteins needed for the fluid lining of the airway.
The study also suggests that RASCs, in addition to their secretory function, serve as predecessors for AT2 cells – regenerating them to maintain the AT2 population and keep alveoli healthy.
Studying lung tissue from people with COPD, as well as those from people without COPD who have a history of smoking, researchers found that in both cases there were many AT2 cells that were altered – hinting at a faulty RASC-to-AT2 transformation.
“With studies like this we’re starting to get a sense, at the cell-biology level, of what is really happening in this very prevalent disease,” senior author Edward Morrisey said.
While the findings point to potential future COPD treatments that may work by restoring the normal RASC-to-AT2 differentiation process, scientists say further research is needed to validate the findings and test this theory.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments