Study reveals how cannabis triggers psychosis
Cannabis is a known risk factor for developing psychosis that can progress to schizophrenia
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Cannabis appears to aggravate already decreasing nerve connectivity in young adults at risk of psychosis, a new study has found.
The study, conducted at McGill University and published in Jama Psychiatry, could pave the way for better psychosis treatments targeting symptoms missed by current medications.
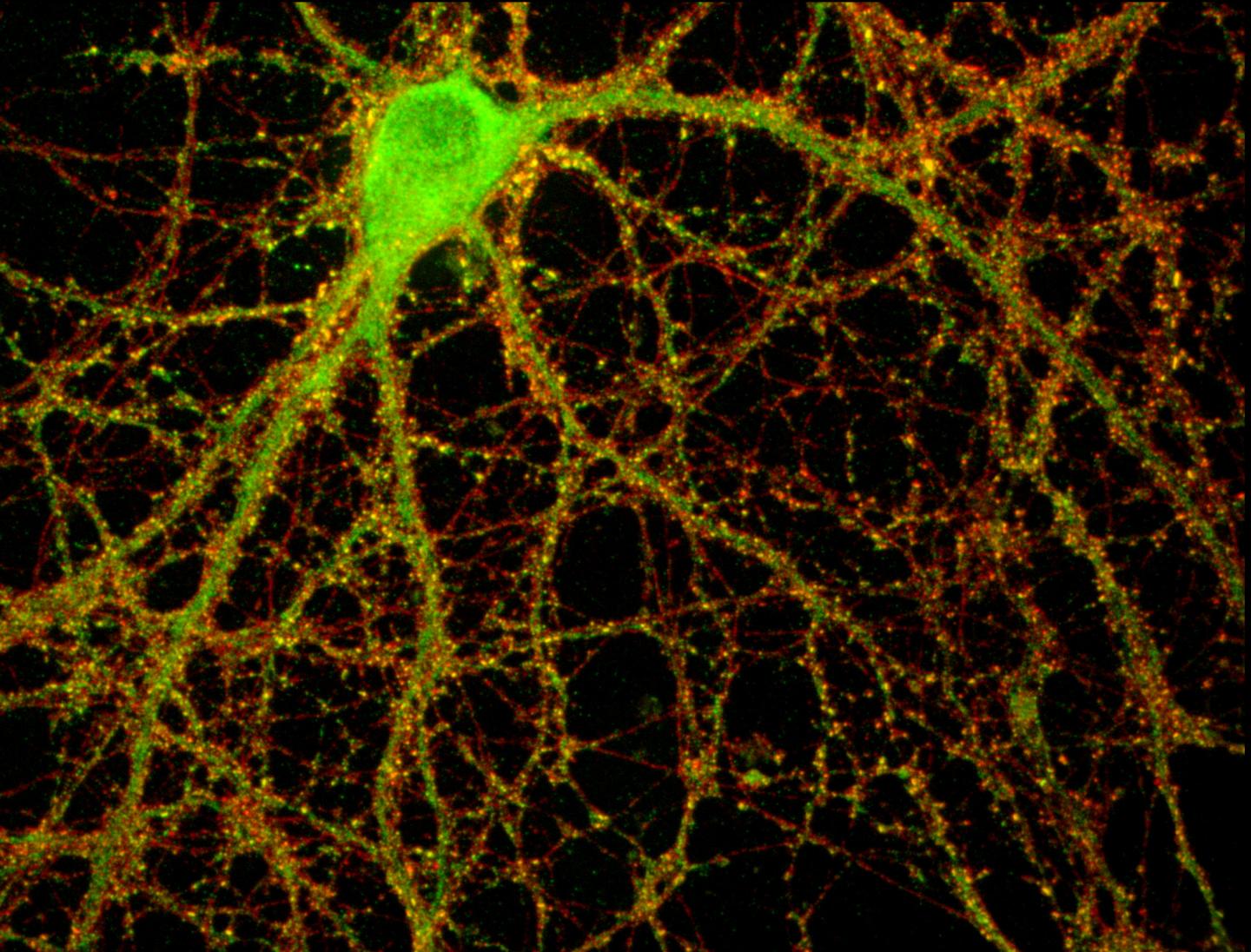
The study detected a marked decrease in nerve cell connections in the brain – known as synaptic density – among individuals at risk of psychosis compared to a healthy control group. Cannabis addiction among these people only exacerbated this process, it found.
Cannabis is a known risk factor for developing psychosis that can progress to schizophrenia but this is the first time researchers have found brain-level changes in an at-risk population in real time.
“Cannabis appears to disrupt the brain’s natural process of refining and pruning synapses, which is essential for healthy brain development,” study co-author Romina Mizrahi explained.
“Not every cannabis user will develop psychosis, but for some, the risks are high. Our research helps clarify why.”
Researchers used advanced brain scanning technology to study about 50 participants aged 16 to 30, including those with recent psychotic symptoms and those considered at high risk.
“This study found that synaptic density reductions were present during the early stages of psychosis and its risk states, and associated with negative symptoms,” the researchers wrote, adding that this dysfunction could lead to schizophrenia.
The scans also reveal that lower synaptic density is associated with symptoms like social withdrawal and lack of motivation, which are considered hard to treat.
Current psychosis medications, researchers say, succeed in targeting hallucinations, but fail at curing these difficult-to-treat symptoms.
“They don’t address symptoms that make it difficult to manage social relationships, work, or school,” study first author Belen Blasco said.
In further studies, scientists hope to explore whether these observed brain changes can help predict psychosis development and potentially enable earlier intervention.
“By focusing on synaptic density, we may eventually develop therapies that enhance social function and quality of life for those affected,” Mr Blasco, a PhD candidate at McGill University, said.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments