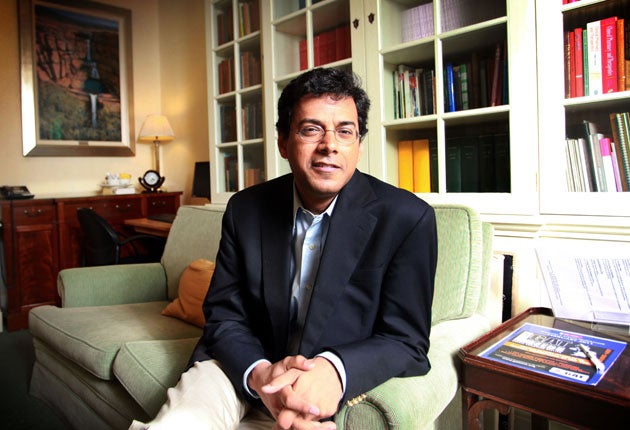
Atul Gawande: a career built on an obsession with deadly failures
The Monday Interview: Atul Gawande is feted by his peers for his dedication to the study of operations gone wrong. Jeremy Laurance reports
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Surgeons are medicine's gladiators, courageous risk takers with big egos, untroubled by self-doubt. We like them that way. You wouldn't want a mouse slicing you open and stitching you up.
But not Atul Gawande. The celebrated American surgeon and writer, who now leads a global drive for the World Health Organisation that promises to save tens of thousands of lives, is made of different stuff. He is, he says, “obsessed with failure.” Instead of celebrating surgery’s 99.5 per cent success rate, we need to examine its 0.5 per cent failure rate. “It is in those margins that thousands of lives are lost,” he says.
A tall gangly figure in crisp blue blazer and cream chinos, he is softly spoken, modest, contained. Yet he creates a buzz wherever he goes. He was visiting England last week, on holiday with his family (“my eldest daughter wanted to see London”) but fitted in a couple of events for Lifebox, a charity he leads (of which more later). The president of one royal medical college, due to attend a dinner in Gawande’s honour, told me he was one of the most inspirational speakers he had heard.
It is for his writing, however, that Gawande, 45, is most admired. As well as his job as a general surgeon at Brigham and Women’s Hospital, Boston, US, he has been a staff writer on the New Yorker since 1998, publishing long explorations of the practise of medicine that have won him wide acclaim.
He has written three books which have become international bestsellers. They are about failure: how it happens, how we learn from it, how we can do better. Although the focus is medicine, the message is for everybody. Against expectations, it turns out to be hugely, enthrallingly optimistic.
Gawande sees medicine from the inside, but with an outsider's perspective. His stories - for he is first and foremost a storyteller - are packed with insights and told with verve and pace.
“Complications”, published in 2002, was written while he was in training. “I tried to understand how I became good at something when mistakes were part of the unwritten and unspoken experience,” he says.
“Better,” published in 2007, involved “trying to understand how anyone gets better” while the “Checklist manifesto” published in 2010, explored “one basic tool that can improve what people do.”
Reviewers have vied to praise him. Geraldine Bedell in the The Observer compared his prose to Orwell’s - “scarcely there, so clear and unarguable is his meaning.” James Le Fanu in the Daily Telegaph, described him as “not just a clever, effortless writer but a morally profound and (dare one say it?) inspirational one.”
Gawande’s message is that instead of denying our fallibility we need to embrace it and learn from it. “People already know we are fallible. What they want to know is that we are aiming for perfection.”
This is as much a moral challenge, as a technical one. It is not about talent - “I don’t believe in talent” he says - but about application, the talent for practice.
“No one looks at your hands to see how much they shake when you are interviewed to be a surgeon. The physical skills required are no greater than for writing cursive script. If an operation requires so much skill only a few surgeons can do it you modify the operation to make it simpler. You want to ensure people can do it right 99 per cent of time. When we have to fire one of our surgical trainees it is never because they don’t have the physical skills but because they don’t have the moral skills - to practise and admit failure.”
How good a surgeon is he? He placed himself in the “mediocre middle” when he was training, he says, but now, in his eighth year of practice, he is “climbing the bell curve.” Like most professionals, he thinks he has recently reached a plateau. Unlike most, however, he is now exploring ways to rise above it - and interviewing tennis coaches, musicians and other performers to find out how it can be done.
It is his readiness to subject his own experience to dispassionate, forensic examination that makes his writing compelling. For Gawande, the sin is not being average, but settling for it. His first New Yorker article, called The Hernia Factory, went through 20 drafts.
He is the son of doctors - his father was a urologist and his mother a paediatrician - but toyed with a political career. There was no direct pressure on him and his sister, a lawyer in New Jersey, to succeed - but it was there indirectly.
“Like all Indian parents there was an expectation that we would get good grades. The importance of aiming for more than mediocre is implanted early. Also, there was the Indian pride in anything you accomplish.”
His first degree in biology and political science at Stanford was followed by a Rhodes scholarship at Oxford where he read Politics, Philosophy and Economics. He returned to Washington to be with Kathleen Hobbs who later became his wife and mother of his three children - they met at college when he was 18. There he worked for presidential candidate Al Gore before finally applying to Harvard to do medicine in 1990.
Midway through his medical school training he again returned to Washington as head of health and social policy for then democratic candidate Bill Clinton, later following him to the White House as a senior advisor. Not for the first time he felt pulled in several directions. He cites a favourite New Yorker cartoon showing a gravestone carrying the legend “He kept his options open.” When he started dating his wife, her mother asked him what he wanted to be. “A professional diletantte,” he replied, adding to me: “It’s worked out pretty well”.
Eventually, to the relief of his parents, he went back to Harvard to complete his medical studies. “I didn’t like the idea of my future being dependent on politics.”
Today he divides his time between surgery and research - looking for ways to make surgery safer. The writing has to be fitted into the gaps - he wrote his first book in the 45 minute “turnaround time” between surgical cases when the operating theatre was cleaned.
Yet the writing is in some ways what matters most - “shining a light on what I do”.
“If I get hit by a bus tomorrow, my patients will not even be postponed. Another surgeon would step in and take over. The reason to do research and writing is that it at least makes me feel not entirely replaceable. If I didn’t write, I don’t know if I would do surgery.”
His interest in ideas spawned what is possibly one of the most revolutionary innovations in medicine of the modern age - the checklist, the subject of his most recent book. It is a list of 19 items, similar to those used by pilots before take off, that need to be checked at the start of every operation, no matter where in the world it is being performed. The checks take two minutes and are extremely basic - is this the right patient? is this the right limb?
The results are remarkable. In four separate studies reductions in death rates of up to 50 per cent and in complication rates of up to a third have been shown. The UK and Ireland were two of the first countries to adopt the checklist which has now been implemented in 4,000 hospitals in 20 countries around the world.
Gawande did not invent the checklist but he developed and popularised it. His argument is that as medicine tries to cope with the advancing complexity of knowledge and treatment, it is falling short in performing even the simplest of tasks. No one person can ensure care is delivered reliably and accurately.
Checklists are now being developed for other areas of medicine including childbirth (being piloted in India), cardiac and neurological surgery, and for the 12 most common crisis situations in operating theatres.
But they have met with resistance from some surgeons who refuse to believe they can be helpful. The checklist requires them to embrace values with which they are not always familiar - including the humility to recognise anyone can make errors however smart they may be. At Derriford hospital, Plymouth, resistance to the checklist resulted in swabs being left inside patients on four occasions last year, triggering a threat of prosecution by the Care Quality Commission, the NHS watchdog. All operating theatres at Derriford hospital are now implementing the checklist.
There is a further problem with implementing the checklist globally. One item - and only one - costs money. The oxygen monitor - a small box that clips to the finger - is used to check the level of oxygen in the blood while a patient is under anaesthesia. Introduced to the UK and US 25 years ago, it saw deaths during surgery fall 100-fold. It is a crucial safety feature but there are 77,000 operating theatres across the world in poorer countries that lack the monitors.
“Before the introduction of oxygen monitors it was not the surgery that was dangerous, it was the anaesthesia. People would suffocate because they were not getting enough oxygen and you wouldn’t know it till their heart stopped. Sometimes surgeons would look up and say ‘why has the blood turned blue?’ That still happens.”
The monitors normally cost up to $2,000 each but by creating consortiums of hospitals to increase their purchasing power, Lifebox has negotiated a deal with a Taiwanese company to make them for $250. One of its first projects will be to distribute them to hospitals in Uganda, backed with training in the operation of the checklist.
For Gawande it is the start of a global push to realise what he has been writing about for a decade - doing things better.
Atul Gawande: a life in brief
* Born in Brooklyn, New York, on 5 November, 1965, Gawande is the son of Indian Maharashtrian doctors. He
graduated from Stanford University in 1987 before becoming a Rhodes Scholar,
earning a degree in Philosophy, Politics and Economics from Oxford.
* After Oxford he embarked on a brief political career, working for Democrat Al Gore before obtaining his MD. He returned to Washington in 1992 as head of health and social policy for democratic candidate Bill Clinton, following him to the White House as an adviser.
* He began writing for the online magazine Slate during his surgical residency, then the New Yorker. His 2009 article The Cost Conundrum was cited by President Barack Obama during his attempt to get the healthcare reform legislation through congress.
* He is married to Kathleen Hobbs, whom he met at 18. They live in Newton, Massachusetts, and have three children.
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments