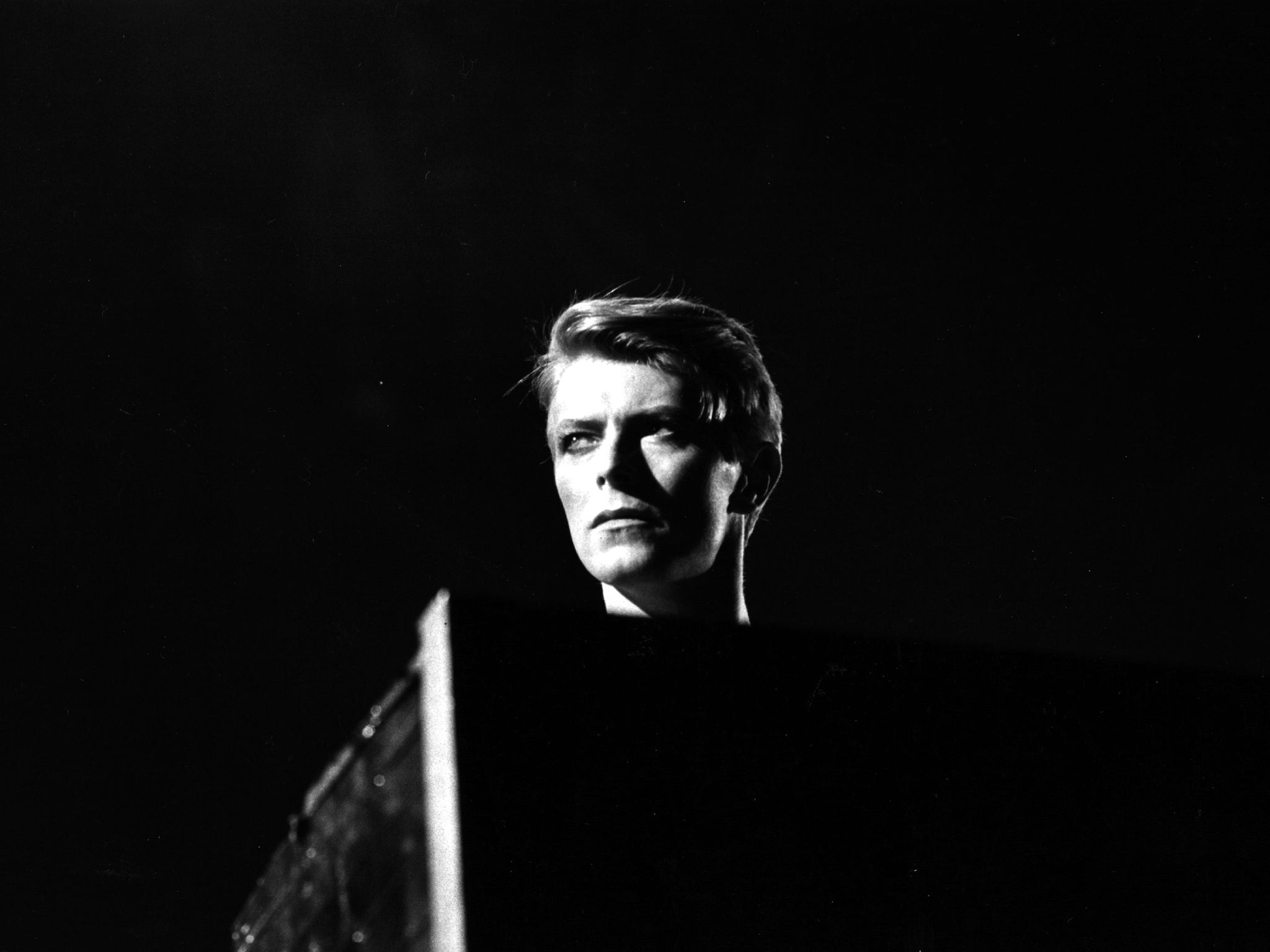
David Bowie: NHS care doctor publishes tribute to the Starman
Mark Taubert was so struck by the choreography of the musician’s final weeks that he published this tribute
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Dear David,
While the realisation of your death was sinking in, many of us went on with our day jobs. For me, that meant a discussion with a hospital patient facing the end of her life.
We spoke of your death and your music, and it got us talking about numerous weighty subjects that are not always straightforward to discuss with someone facing their own demise. In fact, your story became a way for us to communicate very openly about death, something many doctors and nurses struggle to introduce as a topic of conversation.
Thank you for “Lazarus” and “Blackstar” [both from the Blackstar album]. I am a palliative care doctor, and what you have done in the time leading up to your death has had a profound effect on me and many people I work with. Your album is strewn with references, hints and allusions. As always, you don’t make interpretation all that easy, but perhaps that isn’t the point.
I have often heard how meticulous you were in your life. For me, the fact that your gentle death at home coincided so closely with the release of your album, with its goodbye message, is unlikely to be coincidence. All of this was carefully planned, to become a work of death art.
The video of “Lazarus” is very deep and many of the scenes will mean different things to different people; for me, it is about dealing with the past when you are faced with inevitable death.
Many people I talk to as part of my job think death predominantly happens in hospitals, in very clinical settings, but I presume you chose home and planned this in some detail. This is one of our aims in palliative care, and your ability to achieve this may mean others will see it as an option that can be fulfilled.
The photos that emerged of you some days after your death were said to be from the last weeks of your life. I do not know whether this is correct, but I am certain that many of us would like to carry off a sharp suit in the same way that you did in those photos.
You looked great, as always, and it seemed in direct defiance of all the scary monsters that the last weeks of life can be associated with.
For your symptom control needs, you will presumably have had palliative care professionals to advise on pain, nausea, vomiting, breathlessness. I can imagine they did this well, and I envisage that they also discussed any emotional anguish you may have had.
For your advance care planning (by that I mean planning death and care decisions prior to things getting worse and your becoming unable to express them), I am certain you will have had a lot of ideas, expectations, prior decisions and stipulations. These may have been set out clearly in writing, near your bed at home, so that everyone who met you was clear on what you wanted, regardless of your ability to communicate.
This is an area that not just palliative care professionals, but in fact all healthcare workers want to improve, so it is less likely that any sudden health incidents will automatically result in an ambulance emergency admission. Especially when people become unable to speak for themselves.
And I doubt that anyone will have given you cardiopulmonary resuscitation (CPR) in the last hours or days of your life, or even considered it. Regrettably, some patients who have not actively opted out of this treatment still receive it, by default. It involves physical, sometimes bone-breaking, chest compressions, electric shocks, injections and insertion of airways and is only successful in 1 or 2 per cent of patients whose cancer has spread to other organs.
It is very likely you asked your medical team to issue a Do Not Attempt CPR order. I can only imagine what it must have been like to discuss this, but you were once again a hero at this most challenging time of your life. And the professionals who saw you will have had good knowledge and skill in the provision of palliative and end-of-life care.
Sadly, this essential part of training is not always available for junior healthcare professionals, including doctors and nurses, and is sometimes overlooked or under-prioritised by those who plan their education. I think if you were ever to return (as Lazarus did), you would be a firm advocate for good palliative care training being available everywhere.
So back to the conversation I had with the lady who had recently received the news that she had advanced cancer that had spread, and that she would probably not live much longer than a year or so.
She talked about you and loved your music, but for some reason was not impressed by your Ziggy Stardust outfit (she was not sure whether you were a boy or a girl). She, too, had memories of places and events for which you provided an idiosyncratic soundtrack.
And then we talked about a good death, the dying moments and what these typically look like. And we talked about palliative care and how it can help.
She told me about her mother’s and her father’s deaths, and that she wanted to be at home when things progressed, not in a hospital or emergency room, but that she’d happily transfer to the local hospice should her symptoms be too challenging to treat at home.
We both wondered who may have been around you when you took your last breath and whether anyone was holding your hand. I believe this was an aspect of the vision she had of her own dying moments that was of the utmost importance to her, and you gave her a way of expressing this most personal longing to me, a relative stranger. Thank you.
Mark Taubert
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments