More than 100,000 people die from snakebites every year. Why is it so hard to treat them?
Around the world, being bitten by a poisonous snake is a genuine risk – and there’s not enough antivenom to go round. Lea Surugue investigates how scientists are attempting to tackle the problem

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Twenty-year-old Mamadou is lying on a metal cot, eyes half-closed, breathing fast. At his bedside sits his boss, fanning him.
Mamadou is a herder. He guides cattle through large open fields for days on end. A few days ago, having slept outdoors with the cows, he was getting ready to complete his usual route, when a sudden pain in his foot caught him off guard. He had been bitten by a snake.
And not by just any snake: Echis ocellatus, the West African carpet viper. It’s responsible for thousands of venomous bites each year, and is thought to kill more people in Africa than any other species.
Mamadou was first taken to a local health centre, but it couldn’t give him the care he needed. So he was then brought to the regional hospital in Sokodé, Togo’s second-largest city. He’s had to travel over 100km to get here. He was bitten five days ago.
Mamadou’s story is not uncommon, and he is not the only snakebite victim on the ward. Four others have been hospitalised this week in Sokodé, and the hospital is just one of several healthcare centres in the region that deal with snakebite.
Each year, an estimated 2.7 million people around the world are bitten by venomous snakes, and about 100,000 die. Most victims, like Mamadou, live in poor, rural and politically marginalised communities. Data from Africa is fragmented, but the latest figures suggest that snakebite kills up to 20,000 people each year in sub-Saharan Africa alone.
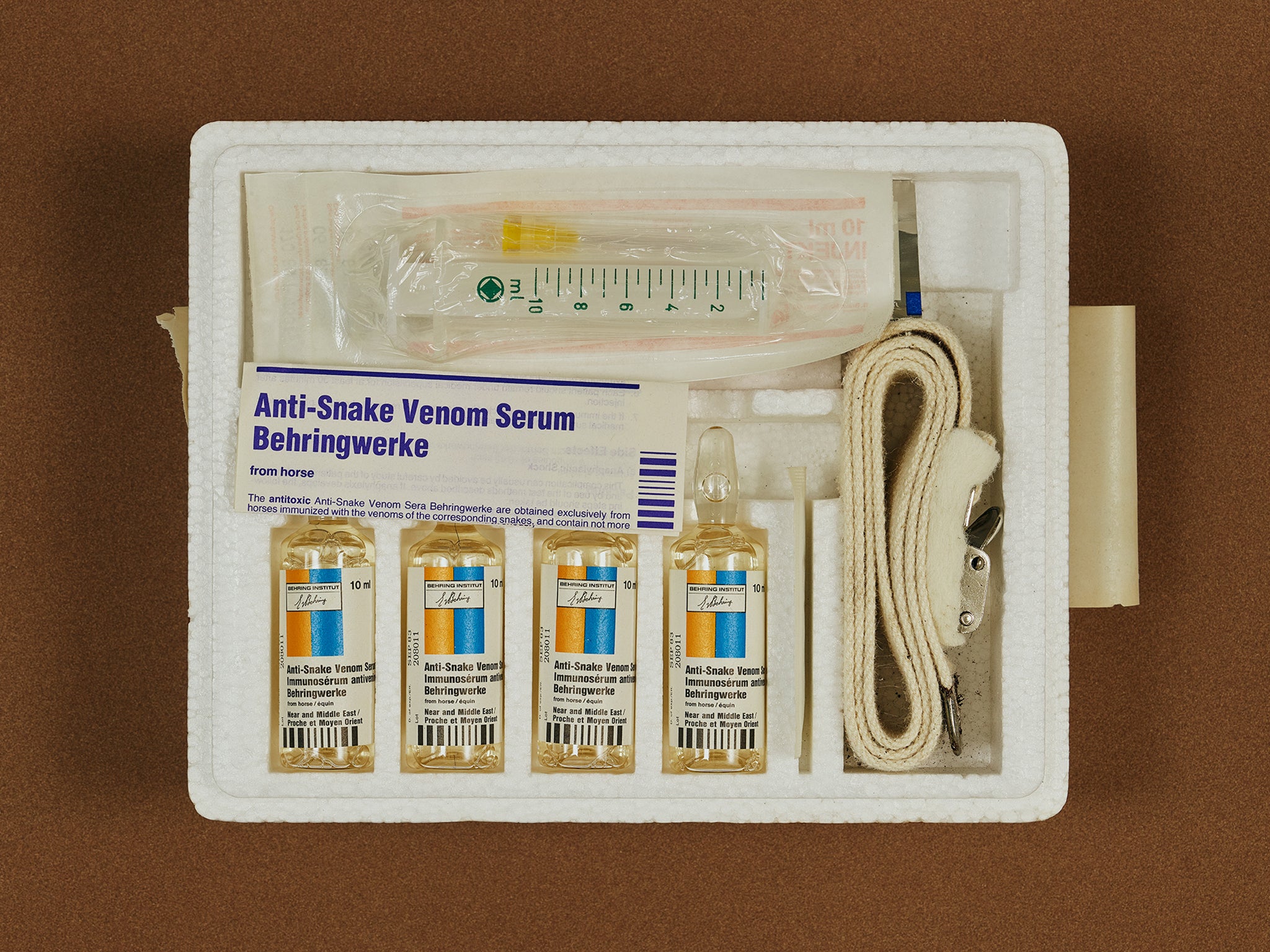
In 2017, the World Health Organisation (WHO) finally recognised the problem by classifying venomous snakebite as a neglected tropical disease. This led to renewed discussions about the only specific treatment currently available – antivenom.
When adequately manufactured, distributed and administered, antivenom saves lives. But right now, the world produces less than half of what it needs. Antivenom is made using a technique that’s over a century old, and there aren’t any common standards to measure its safety or effectiveness, leading to a high risk of adverse reactions. And for over 40 per cent of the world’s snake species, there’s no antivenom whatsoever.
Even when antivenom does exist, it often doesn’t reach the people that need it. Unstable markets have driven up costs, allowing cheaper, substandard treatments to appear. With their patchy efficacy and dangerous side-effects, these are deterring people in low-income countries from seeking treatment at all. Falling demand then makes antivenom even more expensive.
The antivenom field is, in short, a disaster. Snakebite should be a treatable condition. Instead it remains, in the words of former UN secretary general Kofi Annan, “the biggest public health crisis you’ve never heard of”.
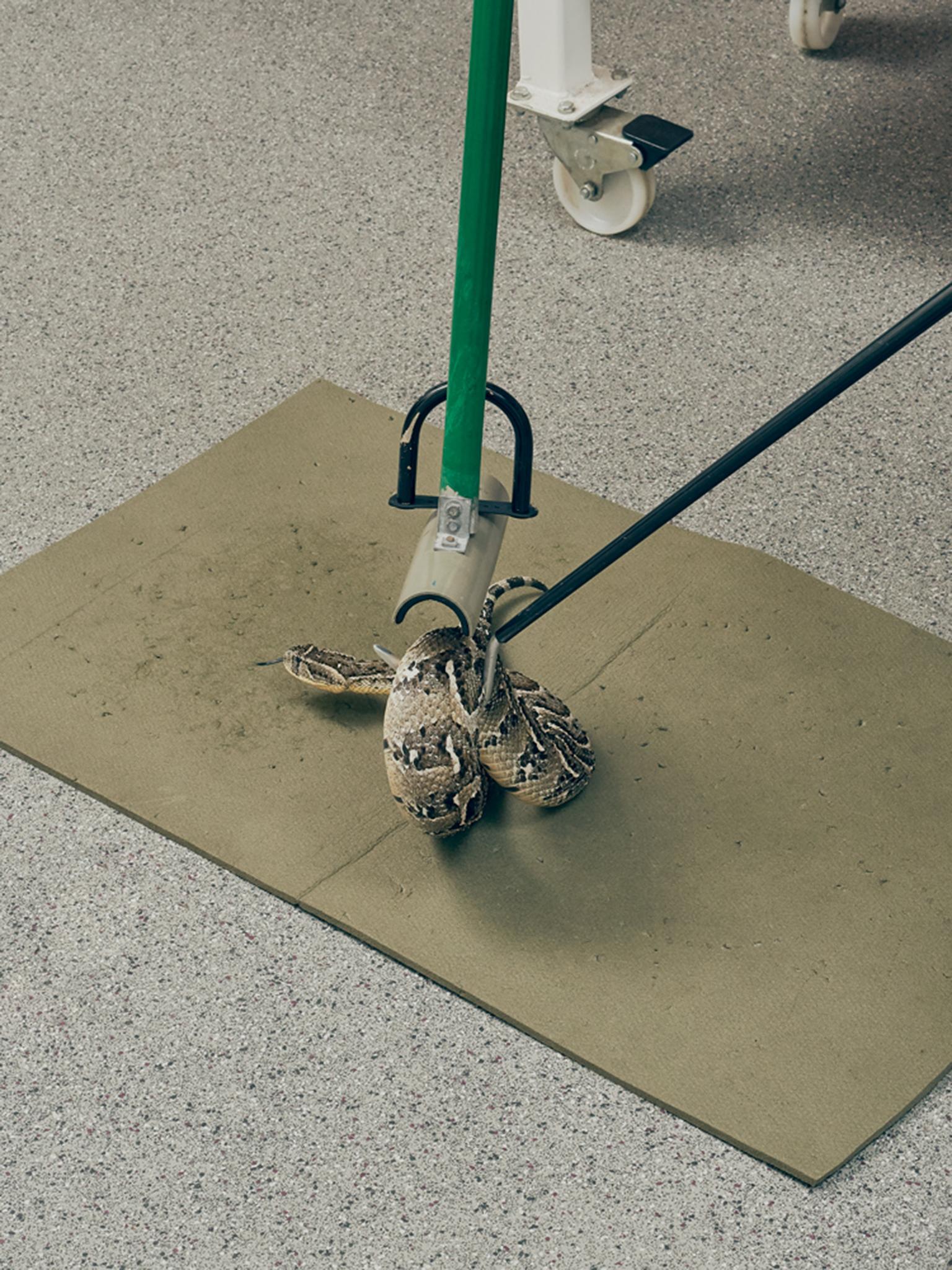
It’s warm where the snakes live. The air in the herpetarium is humid, and on the walls, faded posters sum up the history of antivenom production. The morning is coming to an end, and in transparent boxes, neatly piled up, 163 snakes – spanning 49 different species – are waiting to be fed.
These reptiles, housed here at the Centre for Snakebite Research and Interventions at the Liverpool School of Tropical Medicine, make up the largest and most diverse collection of venomous snakes in the UK. It’s their job is to provide venom for antivenom manufacturers and to help find new ways to treat snakebite.
Today, it’s the turn of the black mamba to be “milked” – that is, to have its venom extracted.
Paul Rowley is the team’s lead herpetologist, an expert in snake handling and husbandry. Slowly, he opens the box to let the mamba out. From behind a large glass window, I follow his careful, deliberate movements as he handles the snake. It’s impressive, a couple of metres long. It’s hard to say if it’s more brown or grey, but it is definitely not black. The snake actually gets its name from the colour of the inside of its mouth.
Despite its length, the black mamba moves surprisingly quickly. Rowley and his assistant have to work together to restrain it, pinning the animal down on the table. Holding its head tightly, they then massage its venom glands to extract the venom as the snake bites on a small container topped with cling film. The whole process takes less than five minutes.
“Most snakes will instinctively bite as soon as they are presented with something,” says Nick Casewell, a research fellow at the centre. “As soon as you move the head of the snake towards a Petri dish, usually they will immediately bite, and you will get venom, too. But it is variable how much venom you get on a particular day.”
Milking a snake is the first step in creating antivenom. The process is over 120 years old, and has changed very little in that time. You inject small, non-toxic doses of venom into an animal – usually a horse or a sheep – to stimulate an immune response. The animal then starts producing antibodies against the venom’s toxins, and you draw some of its blood. Finally, you isolate and purify these antibodies, and make them into a stable solution that can be given to patients as an injection.
This may sound simple, but it isn’t. Because antivenom is made up of animal antibodies and foreign proteins, it can cause adverse reactions in the human body – especially if you don’t purify it well enough. Side-effects range from rashes, nausea and headaches to anaphylactic shock in rare cases.
Venoms are also complicated substances to treat. They’re made up of hundreds of different toxins, whose properties and interactions are still not entirely understood. The combinations of toxins and their effects vary widely from species to species.

Broadly speaking, there are two main families of venomous snakes: vipers (such as the West African carpet viper) and elapid snakes (such as the black mamba). Depending on the type of snake, the toxins contained in the venom can cause different problems, such as damage to the nervous system (more commonly associated with elapid snakes) and bleeding (more common with vipers), as well as swelling and tissue destruction at the site of the bite. Within one venom, distinct toxins can create different kinds of problems.
This diversity means that developing effective antivenom is difficult. An antivenom made using venoms extracted from snakes in one place will have no use in another – and yet many find their way into the wrong markets. Indian antivenom made using local species is commonly found throughout Africa, for example, despite having no effect there.
And even if the right antivenom is available, matching it to a particular snakebite is difficult.
“In at least half of cases, the snake is not seen by the patient,” says Achille Massougbodji, president of the African Society of Venomology. “Even if we have the snake, the skills to identify it are extremely low in regions where bites occur.”
Antivenom can, however, be manufactured to work against more than one type of snake – by immunising horses or sheep with the venom of multiple species from a region. But this “polyspecific” antivenom comes with its own limitations.
In all antivenom, relatively few of the antibodies produced by the sheep or horse are actually specific to the venom’s toxins – studies suggest somewhere between 5 and 36 per cent. In polyspecific antivenom, this figure becomes even lower. “You get a mixture of antibodies that are directed towards different venoms and toxins, and you are only ever bitten by one snake,” says Casewell. “This means only a small proportion of the antibodies in that product are actually against the snake you were bitten by.”
The effect, he says, is that doctors administering a polyspecific antivenom have to use higher doses. This increases the cost of treatment. It also makes it less safe for the patient by raising the risk of side-effects.
In small rural hospitals, concerns over side-effects can leave doctors wary of administering more than one vial of antivenom. In Mamadou’s case, he was referred to Sokodé after being given antivenom so that he could get better follow-up care for the potential side-effects, as well as better treatment for the complications from his bite.
For doctors, finding the balance can be difficult without proper training. Give too much antivenom and you risk side-effects. Give too little, or too late, and it’s not going to work.
In Dankpen prefecture in northern Togo, not far from the border with Burkina Faso, green fields of yams stretch for miles. The rainy season is fast approaching, and dozens of young men are already hard at work picking up tubers from the brown earth. At the side of the road, women are selling cheeses and mangoes, piled up high in their baskets.
In this area, most people work in agriculture, and they are among the most exposed to snakebite. They’re also some of the least able to afford treatment. In Togo, like many countries in sub-Saharan Africa, people have to pay for healthcare out of their own pocket. For many rural workers, the cost is just too great. Around half the country’s households live below the poverty line, particularly in rural areas.
When it comes to snakebite, the country at least fares better than some – the government has recently subsidised antivenom. The Spanish company Inosan Biopharma has also donated 8,000 vials of antivenom, which people will be able to get for free over the next year. However, patients still have to pay for their hospital stay and for other medicines they might need in the course of treatment. And in smaller health centres, antivenom – free or otherwise – isn’t always available.

On a Saturday evening in Dankpen hospital, nurse Amandine Nassimarty is the only person on duty. She is looking after 25-year-old Michel, who was bitten by a carpet viper five days ago while harvesting yams. Curled up on his bed, his arms and legs are covered by thin crusts of dried mud – a treatment he received from the local traditional healer.
Michel has stopped bleeding, but he is still weak. Yet his relatives are asking the hospital to let him go. When they brought him in, unable to speak or swallow due to swelling and bleeding from the mouth, days after the bite, there was no antivenom left to give him. They had to travel by motorbike to the nearest town to buy two doses, costing 37,000 francs each (£50). The legal minimum wage in the country is 35,000 francs a month.
“We have given him two doses of antivenom, but after that, the family didn’t have the means to do more,” Nassimarty says. “His parents are now asking to leave. Patients understand they should stay, but they can’t pay, and often the next day I arrive and they are gone from the bed.”
Togo isn’t the only country where this happens. The price of antivenom may vary depending on the product, but it’s usually too high for families in low-income countries. In India, it’s been reported that treating a snakebite can cost up to 350,000 rupees (£3,900), when on average a farmer earned just over 8,000 rupees a month in 2015/16. When someone gets bitten, family members often have to sell some of their most precious possessions – including cattle and tools – to fund the long journey to hospital and the treatment.
And the cost doesn’t always end there. Snakebite survivors – who are often the main providers for their families – may not be able to work afterwards. A family that pays for antivenom can end up facing economic ruin, and so may avoid treatments in the future.

“Having a rural cattle herder or farmer lose a foot, they might survive, but they become a burden to their families,” says Nick Brown, medical director of MicroPharm, a British antivenom manufacturer. “It’s an unseen toll that people are just not aware of.”
It’s a vicious cycle.
People find that they cannot get effective snakebite treatment – because cost or distribution problems make antivenom unavailable, or because they’ve been given a less effective antivenom, or because their treatment has been given to them the wrong way or too long after they’ve been bitten.
This leads people to stop seeking out treatment, and governments to stop their funding for it, reducing demand and forcing manufacturers to raise their prices. This, in turn, leads to cheaper, less safe, less effective products flooding the market, which the manufacturers of good-quality treatments then have to compete with – or get out of the market altogether.
This happened infamously with Fav-Afrique, one of Africa’s best polyspecific antivenoms. Its manufacturer, Sanofi Pasteur, decided to stop making it because it couldn’t compete with the cost of rival products. Sanofi released its last batch in 2014, which was usable up until its expiry date in June 2016; from that point on, a new manufacturer would be needed. Only in January 2018, 18 months after that final batch had expired, did MicroPharm announce it was taking over production.
At the root of this lies the biggest – and arguably hardest – problem that needs solving: the overall lack of trust in antivenom therapy.
“When nurses and health centres don’t have the right antivenom – or any at all – each time a snakebite happens, it stigmatises a little more this incompetence. People end up considering that the doctors can’t do anything,” says Achille Massougbodji. “There is a lack of trust, which translates into people massively delaying going to consult health services.”
Many patients reluctantly arrive at hospital days after a bite, when they are too sick to be treated properly. When doctors are then unable to help them, this reinforces the idea that they should seek traditional healers first. But the longer people wait to get antivenom, the less benefit they get from it.
However, cutting out traditional healers from a patient’s therapeutic journey may not be the solution.
In the city of Atakpamé, in south-central Togo, a traditional healer sits by the side of the road, minutes away from the local hospital. On a large white sheet tied around two wooden poles, little painted icons show the different ailments he offers to cure. An eye-catching green snake sits in the top left-hand corner.
Sitting on a bench hidden behind the sheet, the old man refuses to give his name. But he is keen to show the plants and the dried-up snake heads and skins that he keeps in boxes, which are part of his therapeutic tools. Gradually, a little crowd forms around him, eager to hear him speak.
The relationship between traditional healers and their communities is deeply based on trust, and this is crucial in the context of snakebite. In many African cultures, being bitten by a snake is seen as something not entirely natural. People sometimes believe it’s a curse.
“There is this whole perception around snakes that means people tend to first go see the person who will not only treat the physical symptoms, but also address the spiritual aspects linked to snakebite,” Massougbodji explains.
So it’s unlikely that people would suddenly bypass their traditional healer to go straight to hospital. Massougbodji believes that working with healers is key – at least by training them to avoid doing things that could make the bite worse, and by getting them to redirect patients to health centres earlier.
However, rebuilding trust between patients and doctors, and getting people to seek antivenom in hospital, will only be possible if health professionals themselves have the right ideas on antivenom.
Jean-Philippe Chippaux, a research director at the Institute of Research for Development in France, knows this all too well. He has been working for decades in Africa on snakebite. He’s come to the northern Togolese city of Kara to speak to health professionals about his experiences, and to share his recommendations on how best to treat snakebite.
Much of Togo is rural, and many of the attendees see snakebite victims on a regular basis, but they never know quite how to react.
Charles Salou*, a paediatric doctor from the south of the country, is one of them. He is quite shaken up by the death of a 15-year-old boy under his watch the week before.
The boy was brought in by a nun, who paid for his treatment. Fearful of possible side-effects, Salou did as he had been taught, giving only one unit of antivenom, even when the boy’s symptoms persisted. It wasn’t enough to have an effect. The boy’s condition worsened, and he died.
Chippaux encounters misperceptions about antivenom’s safety a lot among health professionals. “They either believe it is a dangerous product that is difficult to administer, or that it’s a miracle product that can solve everything,” he says. “But that’s not the case. Antivenom is here to eliminate the venom out of the organism – not to treat the complications that arise.”
Not only do snakebite victims have to receive adequate antivenom, but they may also need to be given other medicines to help with any persisting symptoms. The problem is that little is known about the long-term complications of snakebite envenoming. Internal bleeding, for example, can still occur days after antivenom has been given.
But even if some outcomes can’t be predicted, or even treated, basic training like Chippaux’s is crucial.
“Had I received this training before the arrival of this patient, I could have saved him,” says Salou. “It pains me when I tell myself that.”
Back in Sokodé, Mamadou is getting weaker by the minute. He is suffering from severe anaemia, but the hospital doesn’t have any of the blood products that he needs. A week after his bite, it’s unlikely that more antivenom will help. Doctors are not even sure whether he is still bleeding internally, or if other problems could suddenly appear, making his condition worse.

In Liverpool, Nick Casewell and his team are working to design safer, more efficient types of antivenom – products that are more specific to the venoms that doctors in Togo and elsewhere in Africa are encountering.
The team have broken down the venoms of 22 medically important species from sub-Saharan Africa, to study the specific toxins they contain. They’re trying to understand why venom protein composition is so diverse, and how and why it differs between related species.
At the Technical University of Denmark, associate professor Andreas Hougaard Laustsen and his colleagues are also looking at toxin-specific approaches. Along with the Liverpool group, they are one of the few teams investigating a new type of antivenom made up of mixtures of human monoclonal antibodies that have been grown in a lab.
Generating cocktails of human antibodies is an idea that’s currently attracting a lot of interest. The antibodies used will be carefully selected so that they’re highly specific to important toxins, clearing them out of the body more efficiently than traditional antivenom. They should also be safer to use than animal antibodies.
In 2018, the Danish team were the first to describe the successful use of human monoclonal antibodies against snake venom toxins, in a study published in Nature Communications. The scientists used black mamba venom for their research, which they then broke down into different components, isolating and analysing the toxins.
They then used an in vitro technique called phage display to identify which types of monoclonal antibody worked best against the venom’s toxins. They ended up with a cocktail of three human monoclonal antibodies. When they tested it against the black mamba’s whole venom in mice, the cocktail stopped the venom’s effects.
Elsewhere, Matt Lewin and his team at Ophirex, a Californian pharma start-up, are investigating a small molecule called varespladib. It works by attaching itself to a set of enzymes that are a major common component of snake venom, stopping them from working, and preventing the paralysis, bleeding and muscle destruction they usually cause. Because varespladib molecules are so small, they can work against venom in bodily tissues that antivenom can’t get to.
The team are testing varespladib alone and together with antivenom to see if they can find the best way to use it. They think it might work as a solo treatment in the field, which could be given to patients right after a bite to give them more time to get to hospital. They’ve had some success using the drug to reverse snakebite symptoms in certain animals, such as mice and pigs. They’re now planning clinical trials.
All this innovative research, though promising, will take time to move outside the lab and into the hands of those that need it. “Innovations are very important, but I think it’s very important to balance it with the fact that people are dying right here and now today,” says David Williams, head of the Australian Venom Research Unit at the University of Melbourne and chair of the WHO’s Snakebite Envenoming Working Group.
The antivenom that we already have, if purified and produced following good manufacturing practices, can be absolutely life-saving, Williams says. “It can make all the difference in the world to bringing a person back to living a normal healthy life, as quickly and easily as possible, at the least cost.”
So the priorities over the coming years will be to improve the treatments we already have – including how they’re made – and to make it easier for people to get products that already have a proven track record.
To help, the WHO is currently testing antivenom quality worldwide as part of a “prequalification” scheme. It’s long used this system to assess and maintain the quality of other drugs.
“I think that prequalification exercise will be a game-changer when it comes,” says Ian Cameron, MicroPharm’s CEO. “It will give African governments confidence that they are buying products with a minimum standard, which will drive the other products which are part of the problem out of the market.”
*
A few days after my visit to Sokodé, Mamadou died, probably from internal bleeding caused by the venom.
His case is a stark reminder that antivenom alone won’t be enough to solve the problem of snakebite. The time it took for Mamadou to receive care, and the complications he suffered despite receiving antivenom, make it clear that more research, and better training and health systems are needed too.
The WHO’s envenoming strategy, published in May 2019, acknowledges this. It promotes safe, effective and affordable treatments, but underlines that treatments will only have their best effect if health systems are improved and communities engage with them. Only when patients seek care straight away, with the right knowledge and treatments then being applied, can snakebite be most successfully treated.
But this is possible.
Amavi had been coming back from the market near her home in northwestern Togo when she had her encounter with a carpet viper. It was already dark, and as she hurried home with her packages, she suddenly felt the intense pain of a bite. Thinking it was a scorpion sting – painful but rarely deadly – she decided to get some sleep and wait for the next day before seeking help.
But in the night she deteriorated. She started bleeding from the mouth and from a wound on her leg that she’d had beforehand. Her family realised it must be a snakebite. They rushed her to the local health centre in the morning, but they didn’t have any antivenom. So, wasting no more time, she perched on the back of her father-in-law’s motorcycle and travelled to the hospital in Kanté, 50km away. It took them two hours.
“Two hours is long, but it was relatively soon after the bite,” says Chippaux. “Had they waited more, it would have been much worse.”
The hospital they travelled to is small, and its staff have few resources to work with. But when Amavi arrived, the doctors there reacted quickly. Their reaction, combined with good-quality antivenom donated by Inosan, saved Amavi’s life.
* Some names have been changed.
This article was first published by Wellcome on Mosaic and is republished here under a Creative Commons licence
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments