Motor neurone disease: The hidden cost of the debilitating degenerative condition
People living with the condition often require home adaptations and additional support – but all come at a cost and it frequently falls on already struggling families to foot the bill

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Motor neurone disease can render a person paralysed – locked in a body where they can feel every itch they cannot scratch. The speed of the condition causes costs to rocket, especially when patients become unable to work. Families either spend vast quantities of money or simply go without.
Zeb Nassar, 48, was diagnosed with motor neurone disease (MND) in 2016. Her financial struggle with the disease began when she fell down the stairs on her way out of her flat in Barking, London, and was unable to convince the council to provide her with a stairlift. She was unable to leave her flat for eight weeks, for fear of falling.
“I rang everyone at the council, saying ‘please, I’ve got to get to work’,” she says. “I’m not the type of person who stays home. I said, ‘What’s the solution? You’ve got to get me out.’ They said that there was nothing they could do.”
As time progressed, Zeb began to suffer from depression, and was offered over-the-phone counselling to treat it. She says simply: “I sat on this chair all day long. I just lost interest.”
After lobbying Laila Butt, councillor for Barking and Dagenham, Zeb was nominated for her new wheelchair-accessible flat. The next challenge was the move to the new property – she still had no way to get down the stairs to leave her home for the last time.
Zeb explains: “When I left my old property and I was moving into this flat, I rang everybody to help me get down the stairs. Nobody offered. St John Ambulance would bring me down from this property for £348.
“I took two steps and I just couldn’t do it, I was feeling weak on my legs. I sat on my bum – I went down twenty steps on my bum. I put the pressure on my arms – the next day I could not move. I was so upset it was such a horrible way to leave. I told the council that all I needed was two strong men from anywhere, anybody.”
Issues with diagnosing MND are common. Ammar Al-Chalabi is a professor of neurology at King’s College London, and explains the difficulties that doctors have when faced with the symptoms. “Motor neuron disease takes about a year to be diagnosed on average. This seems to be the same everywhere in the world, regardless of health system, and there are several reasons for it.

“First, although MND will kill one in every 300 people, the average GP sees just one person with it in their working lifetime, and so, very reasonably, they exclude other similar conditions first. Second, there is no diagnostic test, so the doctor has to go through a process of elimination, which takes time. Third, because it is a devastating diagnosis to receive, a doctor will wait until they are very certain before the possibility is mentioned.”
Keith Moore died in May from MND, which he had suffered with for five years. Keith, a former police officer, became aware of having a condition after a fall, but he was initially diagnosed with drop foot before doctors eventually realised that he had the degenerative disease.
Keith lived in Worcester with his wife, and received a full-time care package, which his daughter Karen described as “fantastic”.
Despite the family having care around the clock, the care company would cancel shifts last minute – leaving them scrabbling to change their plans, as they did not have the funds to pay for a private carer.
Karen and her sisters love their father, but were unable to drop everything to look after him when carers did not show up for shifts.
Karen explains that they could not relax. “The agency that we were with are using another agency to get their staff in, but they didn’t know my dad, or understand his complex needs, so somebody would come in and my sisters would have to shadow them because of his complex care. It wasn’t difficult to look after him, but they have to know the equipment that he uses. He was reliant on somebody keeping him alive.”
After a long period of battling with their care company, the family made the difficult decision to put Keith in respite care. However, the decision was anything but simple – in the days leading to his move, they struggled to find anyone who would transport him.
Karen recalls the struggles they faced when trying to move her father: “The system is just ridiculous – I don’t think anyone has thought it out properly … We spent a lot of time on Google and phones, and nobody seems to know.”
In the end, the family used a community bus, a favour which Karen’s sister is waiting to repay back to the community.
When Keith was first in need of a wheelchair, he was provided with a women’s chair, despite being a large man. The family were unable to pay for additional costs, and Karen was frustrated as they would have paid for everything if they could. “We were hoping to build a little wet room, but it’s tiny, you could get his chair in and one carer. It wasn’t suitable but we couldn’t afford anything else.”
Their district nurse works three half days, they just couldn’t get hold of her. “We hadn’t seen her for months and months. She’s got an impossible task, and has been in touch because she heard about what was going on with the care, but it was too late – we’d dealt with it.
“We’ve done a lot of fundraising for MND, and now I just think, if we’d have done that fundraising just for my dad… It’s not just about research, it’s about the care.”
The delay in diagnosis for Bonita Sheehan’s mother Florrie meant she struggled to access the necessary care.
Bonita recalls the difficulties they faced when her mother needed more help around the home, but had not received a formal diagnosis of motor neurone disease. Unfortunately they were unable to pay for the care themselves, and had to make do. “It was as if they thought she was making it up. She did actually get admitted to the hospital in Southampton. She said to me, ‘They think I’m making it up, they really think I’m making it up. If I do die, please make sure you get a post-mortem done because there is something wrong with me.’”
Florrie was a very determined person, and kept trying to live her life as normally as possible. Unfortunately, she kept having falls when she walked, and tried to take her own life twice.
According to research published today by think tank Demos – commissioned by the Motor Neurone Disease Association, the average patient and their family spend almost £12,000 a year on their condition. The findings point to three areas where a person could incur costs: one-off purchases (such as home adaptations), regular expenses (such as care, or additional help around the home) and enhanced costs (such as increased energy bills or travel insurance).
Of the respondents, 82 per cent stated that MND had “moderately negatively impacted” or “very negatively impacted” their finances. Meanwhile, 45 per cent said that the financial support they receive is not adequate. Even at their maximum amount, disability allowances reach £7,337.20 a year – which is a fraction of the average additional cost.
Susie Rabin, head of policy and campaigns at MND Association, explains that there was a huge discrepancy in spending between high and low income families. “We did come across people who had spent high levels of money, and we found people who were struggling to put another £10 on the meter to keep the house heated – who really were going without.
“But we also came across people who had spent hundreds of thousands of pounds adapting their home. Living in a six-bedroom, three-storey house is going to have more significant adaptation costs.
“There’s a lot of money that people can spend – and are having to spend – to be able to live comfortably and safely. I think people want to be able to provide quality of life for them, and be able to enjoy the limited time that they have left.”
Complications with bills can cause huge amounts of stress for families who are already under financial strain. Paul Carrison, 71, was diagnosed with MND two years ago. The disease has since progressed – he is now unable to stand, and is losing strength in his arms. His wife Tina is his carer, but she recently needed to go into hospital for a mastectomy, and was unable to care for Paul due to her stitches.
The couple had made arrangements for Paul to receive six weeks emergency care, which the council said they would pay for. Following this, the couple were billed for the emergency care (this eventually voided) and four weeks additional help which they never received.
Paul says, “We can do without this. At the moment we are hoping to get continuing healthcare as we are really struggling.
“I was diagnosed two years ago and now cannot walk or stand, and am losing strength in my arms. We have a ceiling hoist in the lounge and bedroom, plus a hospital bed for me. We moved last year to a wheelchair-friendly bungalow, which we had to renovate. We were refused a grant for a wet room and had to fund it ourselves with 20 per cent coming from MND Association.
“This cruel disease impacts on the whole family especially my wife who has become my carer, having to wash, dress, undress me and take me to the toilet. Also, she’s now having to flush and turn my peg. I am 71 and my wife is almost 70, at this age the only benefit available is Attendance Allowance. We even had to buy an automatic vehicle and have it adapted to a hand control to enable me to carry on driving, which I now have had to give up.
“Fortunately we have a good support team in our area. Without them and the volunteers I don’t know what we would do.”
Companies seeking to help those struggling with the costs of the condition are popping up across the country. Communication equipment is an area on which family members can spend large sums of money. Patients who rush into buying equipment (perhaps due to delays in receiving NHS equipment, issues with clinical commissioning group funding, or simply wanting to buy the best technology), can be disappointed when the devices do not work for them.
MND Association’s communication aids coordinator, Matthew Hollis, stresses the importance of having an assessment to see which device is best. “Ultimately, nobody should be having to purchase their own communication aid – if the NHS can’t provide it, MND Association will support them if we can.”
Matthew believes that NHS England is providing much more funding for communication devices, but there remains room for improvement. “There are still a lot of people who need support from us as a charity, which may be in the form of financial support or lower tech communication devices.”
Susan Graham started her non-profit organisation, Jaspal’s Voice, in memory of her sister, who died after a 10-year struggle with the disease.
Susan’s goal is to tackle issues with communication devices for patients who cannot speak anymore. On her organisation’s website, it explains the issue: “The NHS provides expensive equipment that cannot be supplied to everyone with the disease. It is left to charities and donors to meet the shortfall. It takes several months before patients are assessed and receive any equipment. Some patients pass away before being supplied with any equipment which is tragic.”
After watching Jaspal lose her voice only a year after diagnosis, Susan was struck by the devastating consequences for someone so sociable. As Jaspal lost the ability to speak, she came up with new and innovative ways to communicate – she could complete a Rubik’s Cube, and would dictate how she wanted family and friends to shift the cube by wiggling her nose from left to right, and her eyes up and down.
Eventually, Jaspal could communicate only by using a large key pad, where she would use predictive text to communicate. Heartbreakingly, on the night she died she sent a simple text reading “goodbye” hours before she passed away.
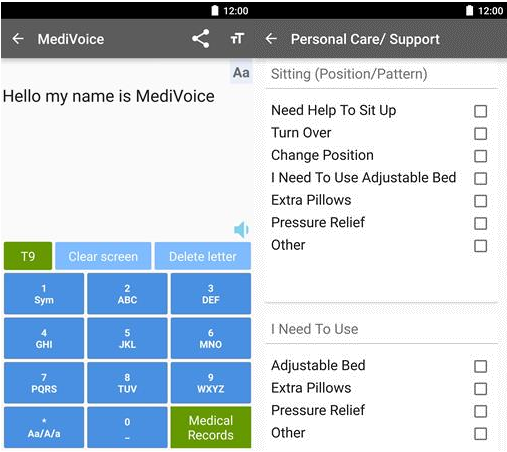
Jaspal’s use of predictive text inspired Susan to create an inexpensive app to suit other patients with MND needs. MediVoice is an app that has a large numeric keypad, which allows for easy predictive texting for those with limited hand movement, but also stores all of the patient’s details to make unexpected trips to the hospital easier.
For example, vital information such as the patient’s most recent blood-pressure readings are stored, alongside more simple – but still hugely necessary – information, such as their likes and dislikes. The app is designed for ease and efficiency, but is also vital when a patient is incapable of speaking for themselves.
In Europe, healthcare for patients with motor neurone disease seems to be better than it is in the UK. Rob Johnson was diagnosed with MND in 2008, after he and his wife Mandy had moved from Warwickshire to France with their five children.
Mandy explains that the system in France is different in that patients are not means tested for expenses such as home adaptations. For example, when the family wanted to renovate their extension to make it accessible for Rob, they were offered an amount that would pay for the basics – if they decided to make the extension more luxurious, they would pay the additional costs themselves.

According to Mandy, the health needs of Rob’s condition are covered 100 per cent by the French government. He has fortnightly visits from his GP at his home, so that he doesn’t go through the stresses of being transported unnecessarily. The British family’s high praise for the European system begs the question: does a similar strategy need to be adopted in the UK?
Rob only has movement in his eyes – meaning that he communicates using a whiteboard with letters written on it. Due to this, he requires around-the-clock care and Mandy is his primary carer, a role she is devoted to. She sleeps on the sofa next to his hospital bed each night, listening to his ventilation device to ensure he is not choking. Mandy champions Rob, ensures he is comfortable when others are treating him, and is his communicator with the rest of the world.
However, despite the benefits of the French system, there are still smaller costs that the family faces. Despite Rob’s healthcare being covered, certain drugs which are not considered as applicable for patients with MND are not paid for by the French health system. In order to prevent Rob from choking on his own saliva, he takes a drug called hyoscine hydrobromide, which comes in patches and inhibits saliva production.
Hyoscine hydrobromide is a drug prescribed for travel sickness, so it is not included in Rob’s treatment package. Therefore, the family shells out €43 (£38) a month on these patches, a cost that can take its toll when neither Rob nor Mandy are able to work.
Another expense is Rob’s bedsheets. They need to be extra strong, so that he can be moved easily between beds, but they are replaced often as they become dirty.
Despite these costs, Mandy refuses to criticise the care that they receive. “We don’t expect to have every single thing paid for. We understand that there is only a certain amount of money to go around for everything.
“We’re getting a lot already, and as lovely as it would be to have everything, and for everybody to have everything, and for every child in school not to be in a class of however many, there’s only so much that they can do.”
With the UK facing an ageing-population crisis, coupled with the expensive and rapid progression of motor neurone disease and constrained resources, the problem does not seem to be disappearing anytime soon.
Chris James, director of external affairs at MND Association, warned that without changes being made, the care made available for patients will become centred around costs, rather than what the patient wants.
He says: “I think that they’ll be doing assessments not based on need, they’ll be setting criteria based mostly on costs, and for someone with MND that may mean if it’s cheaper for them to be cared for in a care home – and it might be – they will be moved out of their home.
“That decision won’t be assessed on their need, it won’t look at them as a person. It won’t be person-centred care, it will be financial-centred care.”
June is Motor Neurone Disease Awareness Month. To find out more about the campaign and the disease see www.mndassociation.org
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments