The Independent's journalism is supported by our readers. When you purchase through links on our site, we may earn commission.
Meet the dogs with OCD
Could understanding canine compulsions help find new treatments for people with obsessive–compulsive disorders, too? Shayla Love investigates
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
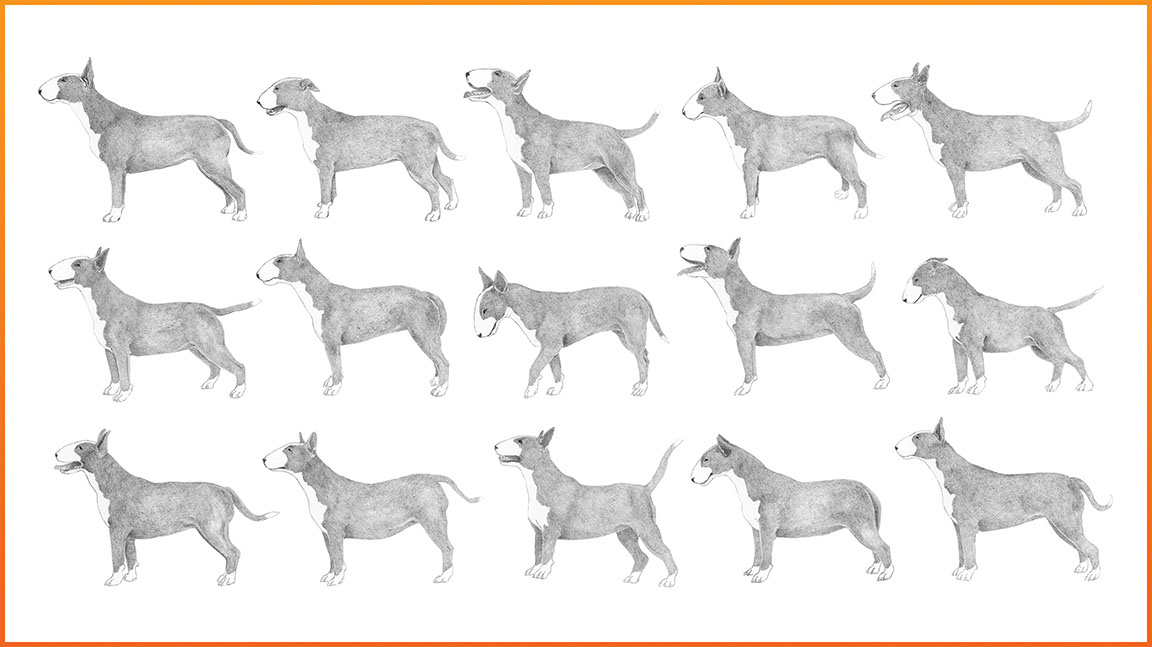
Your support makes all the difference.Curiously, and perhaps eagerly, I am looking at a bull terrier named Sputnik, searching for a resemblance.
He’s a stocky three-year-old, mostly slate grey, with a white stripe on his head and a pink splotch on his elongated, bull-terrier nose. So far, our only similarity is we’re both waiting in a trailer that’s serving as his examination room at Tufts University’s veterinary school in North Grafton, Massachusetts.
Sputnik has canine compulsive disorder (CCD) and is at Tufts for a checkup with Nicholas Dodman, a veterinarian who has been studying CCD for over two decades. I’m shadowing this visit to learn about Dodman’s work and, selfishly, to learn something about myself; I was diagnosed with obsessive–compulsive disorder (OCD) a few months ago.
When Dodman first started seeing these dogs, he realised he had been handed a potentially ideal animal model to study human OCD. But in 20 years of studying dogs, discovering genes that may be involved and new neural pathways, one problem has continually clouded his research: the debate over whether CCD can truly be compared to human OCD. “When it comes to problems of the mind, people have a mental block,” he says. “The mind is thought of as uniquely human.”
I try to see into Sputnik’s eyes. He stays close to his owner, Dan Schmuck, giving me an occasional glance. Sputnik was a tail chaser, and would spin for hours on end. At the moment, he is completely still. Like me, it seems he keeps that kind of behaviour away from the public eye.
Two years ago, after rescuing Sputnik from a shelter, Schmuck went on a business trip. His mother called him to say that their new dog had started chasing his tail, and she couldn’t get him to stop. At first, Schmuck and his wife thought it was funny. They took a video of their young puppy spinning, and you could hear them laughing in the background. But soon, the humour faded.
“It was as if I didn’t exist,” Schmuck explains. “His head will lurch all the way against his shoulder, and stare at his tail, as if his nemesis is staring right back at him. He will slowly start working up to chasing, and it will get faster and faster until his head is hitting whatever wall he bangs into. Even though he’s getting hit so hard that you think he’s getting a concussion, he will keep doing it until his teeth and his tail start hitting the wall and he’s shooting blood all over the place.”
Schmuck had to take time off work to stay home and physically restrain him. He held Sputnik’s head in one hand, and wrapped his arm around his rear until he calmed down or fell asleep. “Then he would wake up and I could just feel him… you could feel his head start lurching like he’s thinking about it. It was an unsustainable situation.”
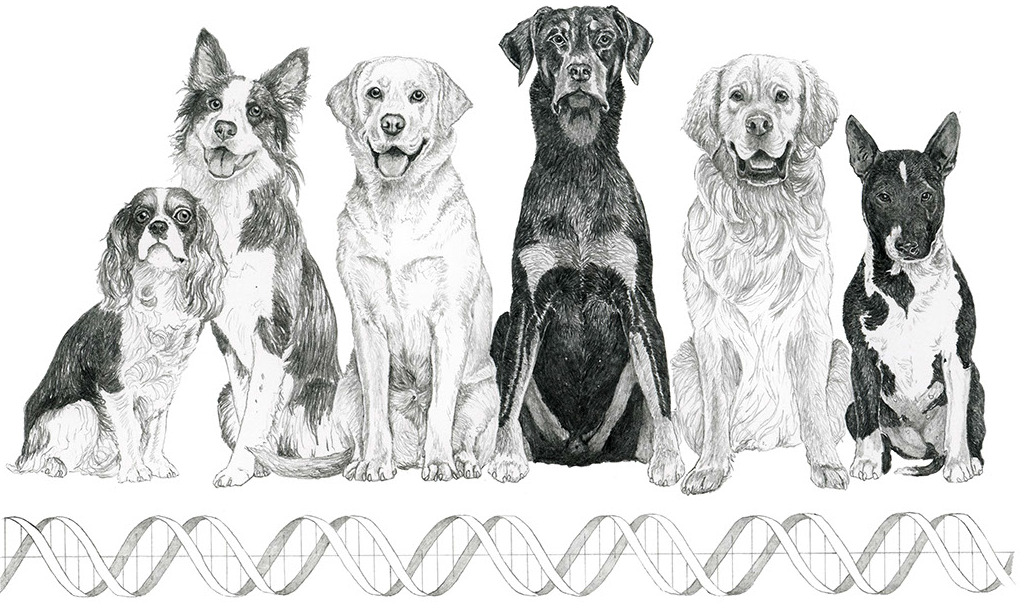
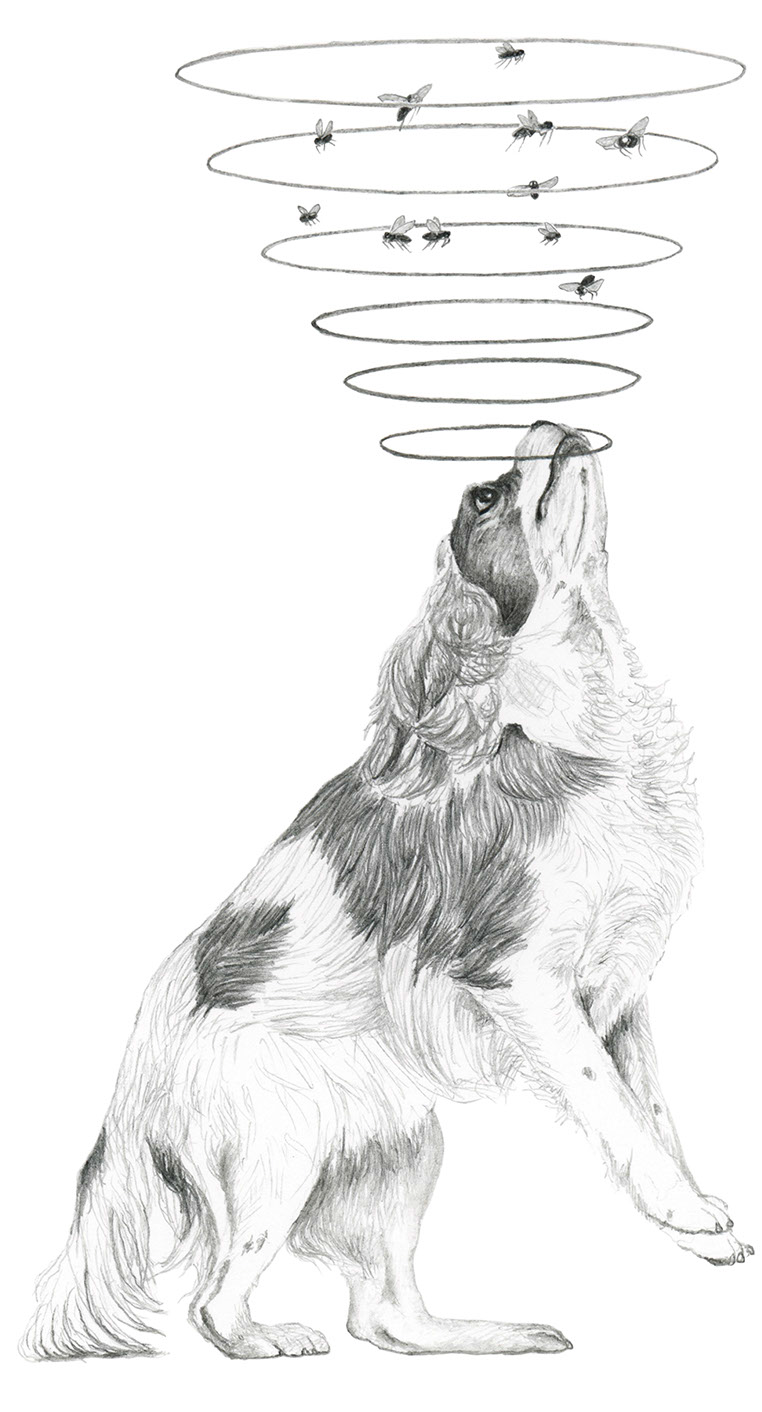
Schmuck drove from his home in Baltimore to see Dodman in Massachusetts. Dodman had seen this kind of spinning many times before. Tail chasing is a common compulsive behaviour for dogs, and for bull terriers specifically. Particular breeds have particular behaviours they exhibit with CCD. Bull terriers spin, Dobermans lick their limbs and suck their flanks, Labradors hold objects or chew rocks, and King Charles spaniels snap at imaginary flies.
Like human OCD, which is commonly focused on washing, hoarding, counting or checking, canine compulsions fit into neat categories. And while these behaviours may sound trivial, they are performed to the extreme. They take over eating, sleeping and all basic functioning. In some cases, they can be fatal.
Sputnik steps out from the safety of Dodman’s shadow, timidly eating treats. His tail hangs innocently between his legs, and I’m having a hard time imagining him whirling, manic, out of control in a pool of his own blood. “Over the last two years, he has gone from being a dog that was going to have to be put down, to being a normal dog,” says Schmuck. “He maybe looks at his tail once a day. It’s a miracle.”
Sputnik is on Prozac now, along with a few other medications to temper his behaviour. Could Sputnik be like me, a person with OCD? Was he thinking about his tail right now, somewhere in the recesses of his doggy mind?
“You can’t access an animal’s thoughts, so the purists call it only canine compulsive disorder, not obsessive–compulsive disorder,” Dodman says. “But it looks for all the world, when Dan is holding Sputnik back, that he’s constantly thinking about it. That’s an obsession.”
*
I was seven, maybe six, when I realised that my hands were dirty. I could wash them, and then they would be clean. But if I touched something – the banister, my clothes, the sofa, a door handle – they would be dirty again. That was easy enough to fix, just wash again. Until, I touched something else, and the process would repeat.
At home, it wasn’t an issue. I could wash my hands whenever I felt my hands weren’t clean. But at school, snack time, field trips – there wasn’t always a place I could wash my hands. Or, the catch-22, the public bathroom at school or the cinema wasn’t clean enough. I couldn’t really be sure that my hands were clean.
I devised a whole bunch of techniques to maintain my hands’ cleanliness. When I went out for lunch on the weekends with my parents, I would wash before we left, close my fists tightly, and hide them in my sleeves until we got to the restaurant. Or I wouldn’t eat the parts of my food that I had held with my hands. I left the bottom halves of French fries and discarded the corners of sandwiches.
I invented a game that I played with my friends at the movies: bobbing for popcorn with our tongues. When the lights dimmed, they returned to eating their popcorn normally; I continued to bob.
This went on for a couple years, until the fourth grade. I still remember the first food I ate without washing my hands. They were fruit gummy snacks handed out at an after-school programme I went to. I opened the plastic bag, reached in with my fingers and put them straight into my mouth. I may have even licked the tip of my index finger a bit. I didn’t know why I was suddenly different, but I felt exhilarated. I was free, normal. I didn’t know what had kept me chained those past few years, but I was glad it was over. I had seconds that day, in my favourite flavour, grape.
*
In 1989, a popular science book called The Boy Who Couldn’t Stop Washing was published. Its author, Judith Rapoport, then chief of the Child Psychiatry Branch at the National Institute of Mental Health, had studied and treated all kinds of neuropsychiatric illness, but a fascination with OCD grabbed hold of her. People with OCD had to participate in detailed rituals and compulsions to assuage strange beliefs: that they had just killed someone, that everything was contaminated, that they had sinned in some way, that things had to be just right.
Before her book came out, OCD was thought to be rare. We now know it affects 1–3 per cent of the population. Rapoport’s book was one of OCD’s first steps into the spotlight – she went on Oprah and Larry King Live. Millions of people began to understand something about their own odd behaviours, or those of their friends and family members. Soon, Rapoport started to get letters and phone calls – including some with questions she hadn’t expected.
“A whole bunch of them talked about their dogs,” she says.
People wrote that their dogs did these behaviours too, especially excessive washing. Did she think they had OCD? It was an interesting idea. “If people ask one weird question, you shrug it off,” she says. “But if 20 of them ask it, you pay attention.”
A dog owner herself, she went to her vet to ask about acral lick, a common CCD behaviour when a dog licks or sucks at its paw or leg until the fur and flesh are worn through, leading to infection, amputation and sometimes death. Her vet told her yes, acral lick was a huge problem with no good treatment options, and his dog suffered from it. She asked if he would be willing to try medication – the same medication given to people with OCD, which increases levels of the brain chemical serotonin.
“We put his dog on a dose that we guessed at, given the weight of dogs and the weight of people, and the dog had a remarkable response,” she said. “You could say this all started when I cured my vet’s dog.”
Encouraged, Rapoport designed a double-blind controlled study. Dogs with acral lick received one of two drugs for OCD that targeted serotonin, or a placebo, or an antidepressant that worked for depression but not OCD and wouldn’t alter serotonin levels. The results were “dramatic”: the only group that improved was the group that got the serotonin drugs.
Still, Rapoport took her findings with a grain of salt. As a psychiatrist, she says she usually needs to know what her patients think of their compulsions to give them a true OCD diagnosis: “Patients with OCD have insight and they say, ‘Look, this is very embarrassing, I think this is crazy what I’m doing, but I can’t stop,’” she explains. “Well, you can’t get that sort of information from animals, so animal models are often very limited for psychiatry.”
After publishing her findings, she moved back to human patients. But her work caught the attention of a veterinary anaesthesiologist with an interest in behaviour: Nicholas Dodman.
*
After an injection of morphine, a small black horse named Knightly Night began to repetitively paw at the ground.
It was the 1980s, and Dodman had noticed that by using different drugs he could change the way animals behaved. In horses, he could “turn on” certain repetitive disorders that in the equestrian world were called stall walking or cribbing. Together with Louis Shuster, a professor of biochemistry and pharmacology at Tufts School of Medicine, he asked the question that would launch his career in animal behaviour: if they could turn a behaviour on, could they also turn it off?
Dodman and Shuster gathered horses with severe problems, who would pace and bite at guardrails, and gave them narcotic antagonists – the opposite of morphine. They all stopped.
“This behaviour has been going on for two thousand years of horses in captivity and nobody knew why,” says Dodman. “We were able to show that somehow you can turn it on and turn it off; that it was caused by some neurotransmitter imbalance.”
Dodman and Shuster’s initial hypothesis was that the drugs were blocking the brain’s natural opiates, stopping the behaviour because the animal no longer felt good while doing it. In further experiments, that theory didn’t hold up. So then they theorised that the on–off switch they had discovered actually lay in the drugs’ effects on NMDA receptors, which interact with a brain chemical called glutamate. Dodman and Shuster thought maybe cutting the line to glutamate was somehow stopping the behaviour.
To test their theory, Shuster went to a local store and bought a bottle of Delsym, a cough suppressant containing dextromethorphan, which also blocks NMDA. They fed it to a pony named Cinnamon Bun, a severe crib biter.
“He glugged it down and it stopped his cribbing behaviour,” Shuster says. “The cough medicine made his lips all pink, he looked rather strange, but it worked.”
Dodman opened an animal behaviour clinic at Tufts to expand his research to other kinds of animals, and the patients began to crawl in. He saw all kinds of pets: more horses, cats and birds, but he began to narrow his focus to dogs.
*
“The reason canine genetics are so cool is one word,” Elaine Ostrander tells me. “Breeds.”
Ostrander is the chief of the Cancer Genetics and Comparative Genomics Branch at the National Human Genome Research Institute, and has been working in dog genetics for 25 years. Her lab develops dog genome databases to look for genes that could be important for animal health or translate to humans. She says they’ve explored everything from infectious disease to cancer, including diabetes, kidney failure, retinitis pigmentosa and gout.
“If you want to understand the genetic underpinning of a complex disease, we know there’s lots of genes involved,” she says. “In human populations, there are dozens of genes that contribute. Every family is a little bit different. Some genes seem hereditary, some seem not to be, it’s a very complex mosaic. In dogs, you simplify that mosaic.”
Within breeds, dogs are genetically very similar. But also between breeds of related dogs, Ostrander can see commonalities. By looking for disease genes in sick dogs in closely related breeds, she can exclude false positives; if four similar breeds with a disease all carry the same gene, one that unaffected dogs don’t have, she knows she’s got a strong candidate.
In 1994, Dodman teamed up with Alice Moon-Fanelli, an animal-behaviour geneticist, to help him begin to explore the genetics of his dog patients. Ostrander had the genetic data and Moon-Fanelli started to gather phenotypes, the expression of those genes: including the details of each dog’s behaviour, along with its breed, pedigree, age of onset, and anything else that might be useful.
Moon-Fanelli says when they started their project, the idea of CCD – not even as a model, just as a standalone disorder – wasn’t widely accepted. Animal repetitive behaviours were considered “stereotypies” – mindless actions that were a result of poor environment or boredom, like tigers pacing in a cage at the zoo. “I came into it asking, ‘Why is this any different?’” she says. “And looking at almost 400 bull terriers over the years, and all the Dobermans and cats, it became clear that it wasn’t because of a suboptimal environment. These animals were pets, they had great lives in wonderful homes.”
The dogs’ symptoms usually started around puberty, as is often the case in people. Compulsive behaviours ran in family lines, just like people. And just as human psychology had to realise that human OCD wasn’t a result of upbringing, animal medicine was doing the same.
“One living species to another, you know that they are obsessing and that they are possessed by demons that they cannot control,” says Moon-Fanelli. “And it’s the same thing with people. It’s just that people speak the same language so they can tell us what they’re thinking. We have to develop our interpretation, and try to be objective, based on what we see in its behaviour.”
Pamela Perry, a behaviourist at Cornell University’s College of Veterinary Medicine, isn’t involved in Dodman’s work. She treats animals that have a variety of behaviour problems, and says that while stereotypies and compulsions can often overlap, she does recognise a distinction. She agrees that we don’t know for sure if animals are obsessing. But she has seen dogs who don’t just compulsively chase light and shadows: they even get up before dawn and wait for the sun to cast shadows that they can then chase. Another client had bought a new washing machine, and their dog would wait for it to turn on and spin along with the whole cycle. As soon as it stopped, he would stop.
“If they’re waiting and anticipating, personally I think we can presume that they’re obsessing to some degree,” Perry says.
*
Despite having one of the classic presentations of OCD, handwashing, it never occurred to me or anyone who knew me that I had OCD. I’ve always been anxious, enough so that I sought out talk therapy several years ago and considered myself a person with generalised anxiety disorder.
My anxieties were always around a common theme: cleanliness, disease, health, germs. I also have a phobia of vomiting, which I obsess about daily. I think about throwing up probably 10–14 hours out of the day, and actively avoid situations that I think will cause me to feel sick or be sick. I thought this was what anxiety was – to be concerned about a specific set of things.
In psychotherapy, we discussed the “reasons” for my anxieties. My parents are scientists and I learned about germs at a very early age. My father was also concerned with germs and cleanliness, food poisoning and food safety. I liked to be in control, and throwing up was a total loss of control, a window into vulnerability. These sessions made me feel better, and I do think my obsessions diminished a little bit as a result. I felt that knowing their origins and roots would help me manage them, help me talk them down.
Looking back, I think my inability to recognise that I had OCD was rooted in the belief that, as a human, I had control over my behaviours and thoughts. Or that, if I didn’t, it was because of deeper human thoughts – if I could just uncover them, I would regain control.
But in situations where I was challenged, I quickly saw how little control I had. When I accidentally ate something that had gone rotten, I descended into total and utter panic for days. When my boyfriend got the stomach flu, I fled our apartment, staying in a hotel for three nights. When I got home, I bought hospital-grade cleaner and bleached and cleaned our home. I didn’t feel safe for weeks; every day I thought obsessively about the germs that were still present, waiting to infect me.
Some of this may sound understandable, albeit a little over the top. But like the dogs, or others with OCD, it’s the amount of disruption of daily life that determines a disorder. I was spending hours upon hours thinking, cleaning, worrying, obsessing.
Throughout all this, I still didn’t think I had OCD, and it wasn’t until my physical compulsions returned, at the end of last year, that I finally thought it might be more than anxiety. I travelled for work from May to December of last year, and dealt with some very minor health problems. Whether through those triggers, stress, isolation, or some combination, the compulsions began to creep back up on me.
Like my childhood handwashing, I don’t know when exactly they began. Now that I’m doing them, it’s as if they’re permanent fixtures, though I can look back six months ago and recognise that I was free of them. My current rituals mostly centre on eating, swallowing and food safety.
Right now, when I eat, I have to eat completely alone, and if someone else is in the room, I cannot eat. I just… can’t. When I do eat, if the food needs to be heated in the microwave, I have to set it to an odd number, usually 4 minutes and 37 seconds. Then, I have to stop the microwave at 37 seconds, though 27 or 17 are acceptable also. (While doing this, I recall with an odd fondness that in my childhood the number on the microwave always had to be 29. It’s like remembering an imaginary friend.) As I’m eating, each time I swallow, I have to lightly touch or grasp the tip of my nose and look up to the far-left corner of my field of vision.
In addition to the eating rituals, my other obsessions got much worse. I started to throw away food compulsively, food I knew – logically – was okay to eat. But fears of contamination take hold: what if it’s gone bad? What if the refrigerator isn’t cold enough? What if this bag of frozen berries was in a place in the freezer where the air didn’t circulate properly?
The fear and obsession with vomiting became extreme. Anything that looked or reminded me of throw-up could cause panic. Spilled coffee, splatters of water, soup, anything creamy, the words ‘chunk’ or ‘throw’. Even writing this single paragraph, using these words, has taken me hours. Each time I write ‘throw-up’ or ‘vomit’, I have to take a break.
Last year, when I was travelling, I wasn’t having any kind of treatment, not even talk therapy. When I got back to New York in January, I enrolled in a clinical trial for people with anxiety at Columbia University. While being evaluated, my interviewers casually asked, “Do you have any phobias or anxieties that aren’t related to your OCD?”
The question stopped me in my tracks. I have OCD?
*
We don’t know exactly what goes wrong in the brain to cause OCD. We do know that a group of drugs known as SSRIs (like Prozac), which increase serotonin levels, seem to help – but only for some people. About half of people see a response to the SSRIs, and a “successful” response can mean as little as a 35 per cent reduction of symptoms. As a recent review of OCD treatments said: “This means that even treatment-responsive patients may continue to have levels of symptoms in the mild-to-moderate range and spend hours daily preoccupied with their obsessions and compulsions.”
Whether you believe in a dog model or not, one thing is becoming clearer in human OCD research: serotonin is not the complete story.
As Dodman had noticed, glutamate seems to be important. Recent neuroimaging of people with OCD has shown higher blood flow and activation in the cortico-striato-thalamocortical circuits, a network that loops from the deep centres of the brain to the prefrontal cortex. This area is dominated by glutamate pathways that are thought to generate controlled movement and thought, and to modulate behavioural routines. Some OCD researchers now hypothesise that SSRIs work not because of serotonin, but because they stop the release of glutamate. Further work, testing the cerebral spinal fluid levels of people with OCD, found that they had significantly higher levels of glutamate.
Still, knowing that glutamate plays a role, in dogs or in people, doesn’t help discover the genes that cause this disorder in humans, which is where an accurate animal model could be extremely helpful.
“The problem with the large number of behavioural disorders is that we don’t really have a good clue as to what the underlying molecular change is,” says Ed Ginns, a neurologist and geneticist who works with Dodman. “If we can at least get that, we’re confident that, with further molecular and clinical studies, pathways and even potential targets for treatment can be identified.”
When he first met Dodman, Ginns had been studying diseases like bipolar disorder and depression in genetically closed populations like the Amish. For him, it was never an issue that Dodman’s sample was built of Dobermans and terriers. He says it was compelling because, like the conditions of those Amish – and unlike other animal models – the dogs’ disorder had arisen naturally.
“These are not artificial constructs,” he says. “These are patients walking into his office with a real behavioural issue. It doesn’t rely on us guessing what we think might be the gene or the change in a mouse that might model a disease.”
Ginns and Dodman’s first collaboration was a genome-wide analysis, comparing 92 flank- and blanket-sucking Doberman pinschers with 68 control Dobermans. They got one strong statistical hit in what Dodman calls a “genetic oasis” – there was only one large gene there for them to look at, called neural cadherin or CDH2. In the brain, CDH2 is involved in the development of glutamate receptors.
“It was a great gene,” Dodman says. “Everyone basically took a big breath and stepped back. This was the first behavioural gene that had ever had anything to do with OCD, and one of the few behavioural genes that have been discovered.”
The next step was to look for CDH2 in people. Dodman and Ginns took their research to the National Institutes of Health, and a group there analysed data they had from people with OCD. The results were inconclusive. They found a suggestion that some CDH2 variants might be associated with Tourette syndrome, but that picture was fuzzy as well.
“We didn’t find something earth-shattering,” says Jens Wendland, a physician and psychiatrist who co-authored the study. “But to be fair, we know now that the cohort would have needed to be much, much larger, at least an order of magnitude larger, to be properly powered to do that. And we tried the best we could with the means we had available at the time.”
Wendland thinks that sequencing has advanced enough that it’s more beneficial to study humans than to redo any dog studies. He is sceptical whether we can ever really be sure that a dog’s symptoms can correspond to humans’. “We will never really know that for sure, so you could argue why should we take this leap of faith in the first place?” he says.
“I would much rather start to work on the biology of genes identified from human studies, however challenging that may be. As opposed to starting with a gene mapped to a behaviour in nonhumans where I can never be certain that this is really affective of the condition that I want to treat.”
*
In 2008, Dodman decided to take the initiative and move his theories to a clinical setting. For many years, he had been discussing his work with Michael Jenike, founder of the Obsessive Compulsive Disorder Institute at McLean Hospital in Belmont, Massachusetts. Jenike enjoyed his talks with Dodman but wasn’t convinced. Like Judith Rapoport, he says that the trouble with dogs and birds and mice is that unless he can talk to them, he can’t properly diagnose OCD. Still, he was willing to try giving some of his patients memantine, a glutamate-targeting drug normally used to treat Alzheimer’s, which Dodman had started giving to dogs with severe CCD.
In a group of 44 patients, everyone got a drug to increase serotonin levels, but half were given memantine as well – and it worked. For those who also got the glutamate drug, symptoms reduced by 27 per cent on average, compared to 16.5 per cent for the others. It isn’t perfect, but Jenike continues to use this combination of drugs with patients who aren’t responding well to SSRIs. Dodman and Shuster had already patented the combination of drugs as a treatment for OCD, but their tech transfer office at Tufts couldn’t get any pharmaceutical companies interested. However, subsequent research has supported the idea that both serotonin and glutamate pathways need to be addressed when treating OCD.
In brain imaging of his compulsive Dobermans, Dodman found that they had structural abnormalities associated with OCD in humans. In February 2016, a group led by Dan Stein, head of the Department of Psychiatry and Mental Health at the University of Cape Town, published the results of a re-examination of the CDH2 gene in humans. Their sample was made of 234 people with OCD and 180 healthy controls, and their findings were more conclusive than the previous study: they found two differences in the CDH2 gene that seemed to be correlated with OCD, though Stein says more work is needed to fully understand the connection.
Dodman’s latest work, published in 2016, compares dogs that have severe and mild cases of CCD. He found two areas of interest in the genome. The first has a human counterpart that is associated with an increased risk of schizophrenia, and the other harbours serotonin receptor genes.
From these most recent findings and their connection with serotonin, Dodman has a new theory. He thinks that the CDH2 gene, which involves glutamate, is required for a dog to be genetically predisposed to CCD in the first place. A human might have a different predisposition gene, but Dodman guesses it involves glutamate too. Serotonin genes, he thinks, are modifiers that control to what degree a dog has CCD (or a person has OCD). He now hopes that someone will look for similar modifier genes in humans, or expand standard OCD treatment to include both serotonin and glutamate pathways.
Dodman still thinks that any hesitation to accept research based on a dog model of human OCD doesn’t lie in specific doubts about the validity of the model, but in a greater philosophical problem: the difficulty in accepting that our minds might be closer than we want to believe to the minds of dogs.
“It really helps to be a veterinarian,” he says. “Because one of the things people say when you’re a vet is, they say: ‘It must be so difficult because you have to learn all these differences between the various species.’ The answer is, actually you don’t. What you learn to do is appreciate the sameness.”
*
As my evaluations at Columbia have continued, I’ve come face to face with another kind of sameness. It’s unsettling, almost spooky – as if someone has entered the most private, most anxious parts of my brain, written down my personal thoughts, and then put them on a questionnaire to be read out loud by a bored psychiatrist. Every worry, every obsession, the things I have to do in secret are standardised and stereotypical enough to be on these general evaluation forms.
Soon after I was officially enrolled in the clinical trial, I began cognitive behavioural therapy (CBT). It is the exact opposite of my past therapy sessions. I loved my psychodynamic therapist. We would meet once a week in her pleasant office, with bookcases and Asian artwork hanging on the wall. She was achingly smart and well read, and as we talked about my feelings and childhood, we often discussed theories and psychoanalytic texts. It felt like an intellectual exchange, something human of the highest order. Deconstructing, understanding, breaking down symbols and metaphor into meaning.
At CBT, I am meeting twice a week on a hard plastic chair in a tiny office with no windows. But we are not here for my feelings; actually the opposite. I am here to provoke my anxieties, confront them and, hopefully, neutralise them. I’m beginning exposure therapy and response prevention. We will not be discussing my dreams. CBT feels as close to dog training as any human activity can get.
We meticulously go through all my phobias, obsessions and rituals and rate them on a hierarchy. Now my job is to attempt to cease the rituals, and expose myself to increasingly upsetting stimuli for an hour a day, and 90 minutes twice a week in session.
After my first exposure session, I was stunned the whole subway ride home. It was upsetting, but more because it was the first time I realised how sick I was. I had looked at photos of spilled orange juice, something I haven’t been able to do because it reminds me of throw-up. First I looked at a cartoon, then more and more difficult photos (difficulty being based on how similar the colour and texture were to actual vomit).
I was so distressed by these photos I could barely glance at them before breaking out into my touching-and-looking swallowing ritual. There was a part of me that thought: this is ridiculous. It felt as if I was being tortured, but I was simply seeing a cup of juice overturned. How could this be making me so upset? I knew it was a cup of juice, and yet when I looked at it, the obsessions flowed in, thinking about being sick, thinking about if the image would make me sick, imagery of me or others getting sick, on and on.
Alice Moon-Fanelli said that the spinning dogs seemed like they had been taken over by demons. These were my demons. I didn’t expect them to look like spilled juice.
I picked up a copy of Rapoport’s book, now over 25 years old, and the same Twilight Zone-esque feelings from my evaluation interviews came back. The young boy who “couldn’t stop washing” also hid his fists in his sleeves and had a complicated swallowing ritual that involved touching and blinking. If the name had been removed, I could have easily believed someone wrote it about me.
In her book, Rapoport wrote that she was amazed at the sameness of OCD behaviours. Though she remains unconvinced how much animal models will ultimately help, she did say that psychiatrists could learn from the work of ethologists, who study inborn behaviour patterns in animals. Rapoport’s collie dog turned in circles – not compulsively, but before it lay down to sleep. In the dog’s ancestors, that behaviour was conserved to trample down grass or ward off hiding snakes or insects. But in her suburban home, it remained.
“The highly selective nature of OCD behaviors is just as remarkable,” she wrote. “Washing, grooming, hoarding – any theory of this disease must account for the incredible selectivity of these behaviors, which could be action patterns from an ethologist’s field book. As psychiatrists, we need to be field observers much more often than we are.”

Forcing myself to see myself as an animal, one that could be overtaken by innate behaviours, helps me make sense of what it means to have OCD. The endless thoughts of vomiting and cleanliness, and my eating rituals, are the same as a dog spinning round and round. The spinning even provided me an apt visual metaphor to latch on to. When the thoughts or fears begin, it is like a whirlpool: swirling, spinning, gaining momentum and sucking all logic or reason into the bottom, out of sight. As a human, I am enraged when I can’t stop my obsessive thoughts. As an animal, it makes sense that I can’t talk my way out of compulsions or fears. It is easy to accept that a dog’s broken neural circuitry was causing their tail chasing. I’m working on lending myself that kind of compassion.
*
The day after Sputnik, I meet Bella, another bull terrier who used to spin but after treatment has stopped almost completely. Bella’s owner, Linda Rowe-Varone, has a similar tale to Sputnik’s owners: one day her sweet puppy started to spin, and nothing she could do could stop her. Like Dan Schmuck, she tells me she almost reached breaking point.
“There was a time I really thought she was spinning so much that I could not keep her in my home anymore,” she says with tears in her eyes. “And Dr Dodman just kept telling me, ‘Just wait it out, wait it out, you’ve got to give her a little more time.’ And I’m really glad I did.”
Bella is active, playing and running around the examination room. Rowe-Varone tells us that Bella is also obsessed with balls, and she has to limit what kinds of toys she is exposed to. I wonder where the vets draw the line? All dogs have a favourite toy, one they love to play with. When can they call it an obsession? (When did I go from being a person who liked to be clean, to becoming obsessed with cleanliness?) Rowe-Varone says that she has to keep balls hidden in the garage, and if Bella sees them, she will sit outside the garage door for hours.
The debate about whether dogs can truly obsess doesn’t enter this room. The consensus here is that Bella knew her balls were in the garage and couldn’t get them off her mind. I’m struck by how accepting dogs as an animal model for human OCD required two shifts in thinking: not only did we have to become more animal, but we had to grant them a bit more humanity as well.
Dodman remembers a dog that was obsessed with water. It lived mostly in New York City but when it went to the owner’s Hamptons home it would jump into the pool and do laps for seven hours a day, whining in anxiety the whole time.
Stephanie Borns-Weil, who took over from Dodman as programme director at the Animal Behavior Clinic at Tufts last year, has seen a golden retriever obsessed with water too: it would get into the bathtub with the kids, or stand in puddles on its walks and refuse to move. Another dog she saw a few months ago would go into a lake by its house, take out five rocks and put them by a tree. If the owner removed them, it would return to the lake and get the rocks back.
One Doberman needed to cover her food before she ate. When her owner fed her, she put some paper towels next to her food. The dog would take a paper towel very delicately in her mouth, cover the food, and then uncover the food to eat it. If she couldn’t perform this ritual she wouldn’t eat. Dodman remembers another odd eating ritual: a dog who would take individual pellets of food and place them in the button compressions in the couch cushion in the next room. Only when he had put seven pellets into seven button holes could he eat the rest of the food out of his bowl.
I look back at Bella, who has bored of our chatting and is resting underneath a desk. The eating rituals that Dodman and Borns-Weil are describing are hitting a bit close to home, and maybe that’s why, for the first time, I do recognise a bit of myself in Bella. There is a big container of balls above her head, which we hurriedly covered when we came in. Is she thinking about them now, just like I’m thinking about my own obsessions?
When I leave Tufts that day, my boyfriend, Zach, picks me up and we head back to our hotel, tired and hungry. I don’t have a driver’s licence, and I needed Zach to drive me the three hours to rural Massachusetts. The drive up from Brooklyn was fraught with anxiety. Being in the car is one of my triggers. Obsessions about car sickness began weeks ago, when I first booked the rental. The whole drive I was tense and white-knuckled.
I know that I need to eat the moment we get back to our room. Zach jumps on the bed, settling in with a book. Nervously, I ask him: can you leave, so I can eat? The ritual needs to happen alone. He’s frustrated. Now? He will have to go sit in the lobby. Fine. Annoyed, he grabs his coat and heads towards the door.
Now I’m upset. Upset I have to do the ritual, upset he can’t be more understanding, mad at myself for having so little control. “You think I want to do this?” I yell defensively. “I just need a little time.”
“Whatever,” he says, slamming the door.
I realise I’ve made the same plea Dodman made to Rowe-Varone when she was about to give up on Bella: “You’ve got to give her a little more time.”
I’m in tears as I set up for lunch. Three napkins, an odd number, and I warm up the soup stopping on 37. I eat, with the ritualised looking and touching, trying to not think about how my soup kind of looks like throw-up.
“It’s not that they’re dogs and it’s not that we’re humans,” Ginns said to me. “It’s that both groups are suffering from this same clinical presentation that disrupts their development and lives. And it’s that description that for me defines compulsive behaviour.”
I take a deep breath. Just wait it out, wait it out, you’ve got to give yourself a little more time.
This article was first published by Wellcome on Mosaic and is republished here under a Creative Commons licence.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments