Antibiotic-resistant superbugs caused 1.2 million deaths in a year, study finds
Study makes comprehensive estimate of the disease burden for 23 microbes and 88 pathogen-drug combinations
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Antibiotic-resistant infections have killed over 1.2 million people in 2019 and emerged as a leading cause of death worldwide, according to new research.
A better estimate of the true scale of antibiotic resistance worldwide was provided by the research, published in The Lancet journal on Thursday.
It showed the number of deaths had exceeded the number of fatalities caused by the likes of HIV/AIDS and malaria.
The research also makes a comprehensive analysis of the disease burden of superbugs and calls for immediate action to find new strategies that can help reduce this burden.
Over the past few decades, bacteria have developed resistance to antimicrobial drugs used to treat their infections and have emerged as one of the leading public health threats of the 21st century.
Some estimates, including the Review on Antimicrobial Resistance commissioned by the UK government, said antimicrobial resistance (AMR) could kill 10 million people per year by 2050.
Based on the current analysis, researchers said there were an estimated 4.95 million deaths linked to superbugs in the year, including 1.27 million deaths attributable to bacterial AMR, making it the third-largest cause of death in 2019.
“Only ischaemic heart disease and stroke accounted for more deaths that year,” the scientists wrote in the study.
This number was nearly the same as “global HIV deaths (680,000) and malaria deaths (627,000) combined, and ranks behind only Covid-19 and tuberculosis in terms of global deaths from an infection,” according to epidemiologist Ramanan Laxminarayan from the Centre for Disease Dynamics, Economics and Policy in Washington.
“The study’s estimate of 4.95 million deaths associated with bacterial AMR globally in 2019 indicates that there are substantial gains to be made from preventing infections in the first place,” Dr Laxminarayan, who was not associated with the study, pointed out in an editorial about the findings in The Lancet.
Lower respiratory infections, according to the study, accounted for more than 1.5 million deaths linked to AMR in 2019, making it the most burdensome resistance-related syndrome, closely followed by deaths due to such infections in the bloodstream and intra-abdominal infections.
Western sub-Saharan Africa – a region that includes Cameroon, Nigeria and Gabon – has the highest death rate attributable to drug resistance at 27.3 deaths per 100,000 people.
This indicated the highest burdens were found in low-resource settings.
“Our analysis showed that AMR all-age death rates were highest in some lower-middle-income countries (LMICs), making AMR not only a major health problem globally but a particularly serious problem for some of the poorest countries in the world,” the researchers added.
While previous studies have attempted to calculate the global burden of antimicrobial resistance, scientists said these estimates were challenged by unreliable data on drug resistance exhibited by microbes and the difficulty of attributing the death burden to AMR specifically.
The researchers, including Christopher Murray from the Institute for Health Metrics and Evaluation (IHME) at the University of Washington, made a comprehensive estimate of the disease burden for 23 pathogens and 88 pathogen–drug combinations in the new research.
They included data from systematic literature reviews, hospital systems, surveillance systems and other sources covering 471 million individual records across 204 countries and territories in 2019.
The analysis distinguished between drug-resistant infections replaced by drug-susceptible infections – infections that can be treated more easily with drugs – and resistant infections that were replaced by no infection.
In the first case, deaths would not have occurred if these infections had been drug-susceptible and in the latter, while AMR is implicated in death, drug resistance itself may not have been the direct cause.
This approach has helped more clearly address the actual difference between disease burden directly attributable to AMR and burden linked to drug resistance.
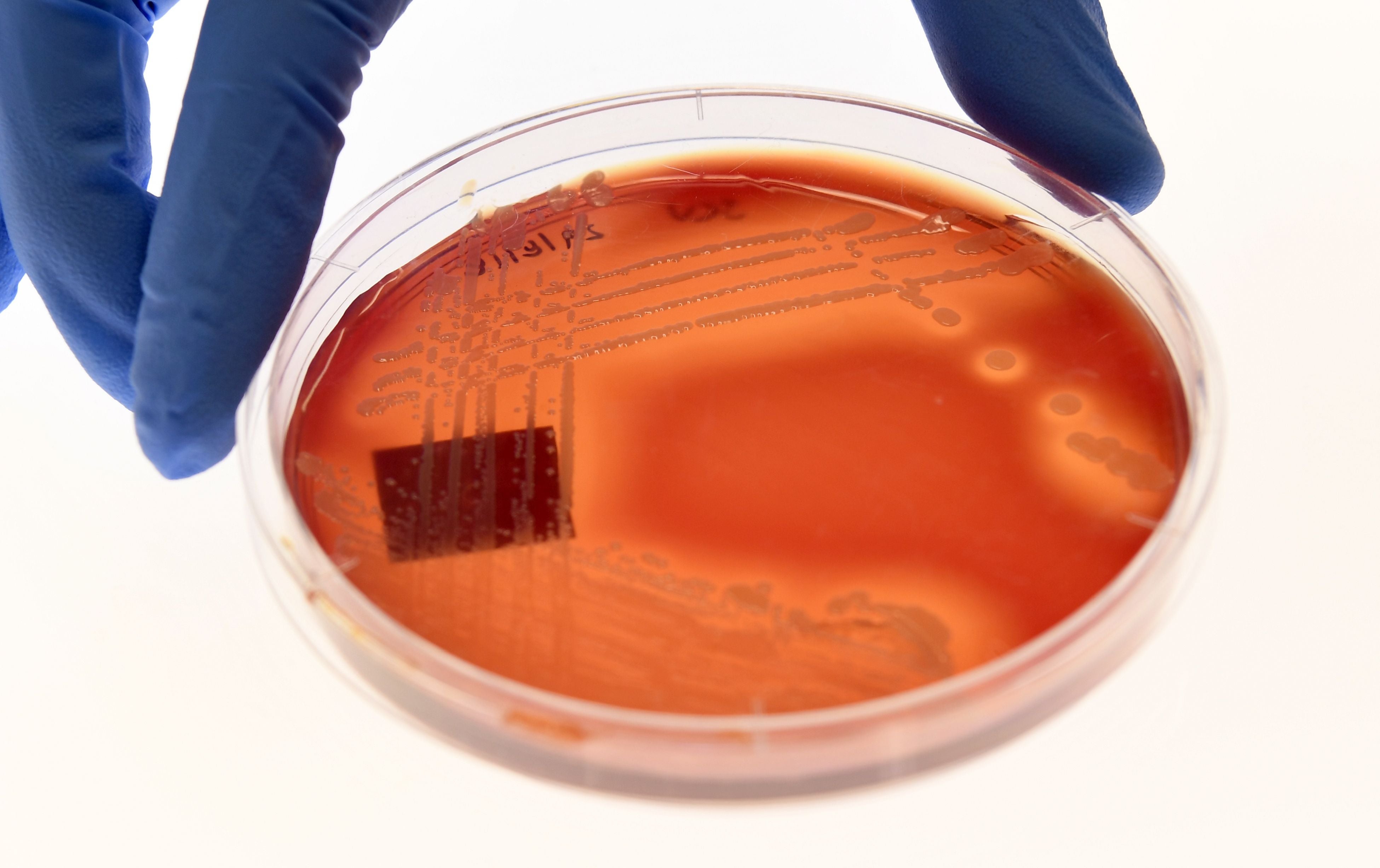
The study also noted that the six leading pathogens which caused deaths associated with drug resistance were Escherichia coli, followed by Staphylococcus aureus, Klebsiella pneumoniae, Streptococcus pneumoniae, Acinetobacter baumannii and Pseudomonas aeruginosa.
These six bacteria, the researchers said, were responsible for 929,00 deaths attributable to AMR and 3.57 million deaths associated with AMR in 2019.
The S aureus bacterium, resistant to the drug meticillin, alone caused more than 100,000 deaths attributable to AMR in 2019, the study noted.
Multidrug-resistant – excluding extensively drug-resistant – tuberculosis, third-generation cephalosporin-resistant E coli, carbapenem-resistant A baumannii, fluoroquinolone-resistant E coli, carbapenem-resistant K pneumoniae and third-generation cephalosporin-resistant K pneumoniae, each caused 50,000 to 100,000 deaths, according to the study.
Five types of strategies were enlisted to address the challenge of bacterial AMR, including infection prevention and control programmes, vaccinations, developing new antibiotics, minimising their use, and reducing use of the drugs in scenarios unrelated to human sickness such as in poultry and animal husbandry.
“Increased use of antibiotics in farming has been identified as a potential contributor to AMR in humans, although the direct causal link remains controversial,” the study noted.
The researchers pointed out that combatting the AMR scourge requires both global action and nationally tailored responses as a “one size fits all approach might be inappropriate”.
Expanding the analysis to more pathogen–drug combinations – adding viruses, parasites and fungi to the calculation – would increase the estimate of the disease burden from AMR, they added.
While the researchers said the study had some limitations, including the lack of data on bacterial infections and resistant pathogen-drug combinations in some parts of the world, they believe the findings can still be used to better inform treatment guidelines.
“The dominant bacterial pathogens for a given infectious syndrome and the antibiotics that would offer effective treatment could be identified using the data for this study, which, along with estimates of pathogen–drug burden, could be used to inform empirical syndromic treatment guidelines tailored to a specific location,” they added.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments