Black people have highest rate of STIs in Britain. Not enough is being done to change that.
Black Britons have ‘disproportionally high rates’ of various STI diagnoses compared to white Britons
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Black people have the highest rate of sexually transmitted infections in Britain and officials are not doing enough to address the issue, sexual health experts have warned.
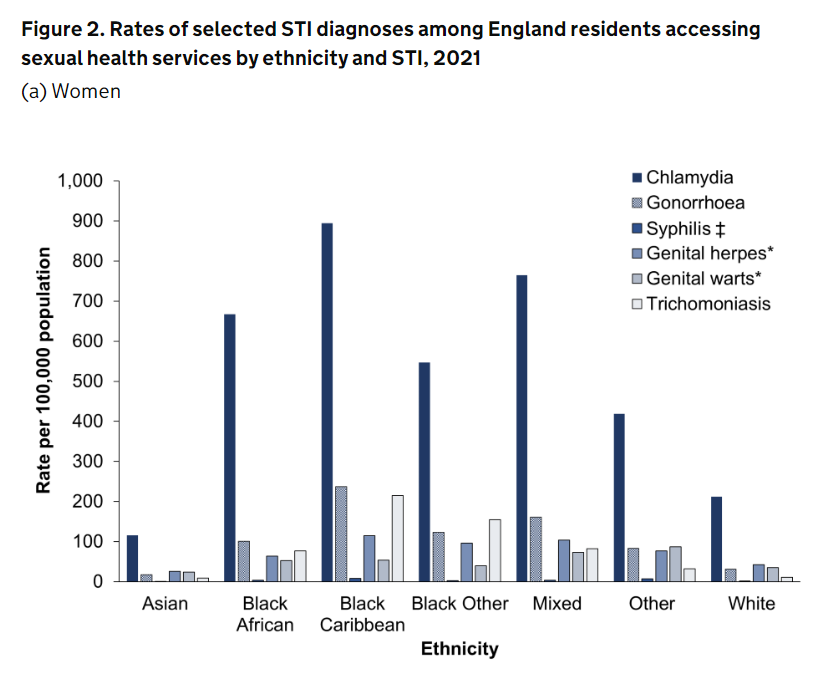
Black Britons have “disproportionally high rates” of various STI diagnoses compared to white Britons, with those of Black Caribbean heritage specifically having the highest rates for chlamydia, gonorrhoea, herpes and trichomoniasis.
Experts have told The Independent that healthcare providers are failing to address these disparities in STIs. They have called for more research to fully understand the complicated reasons why STIs are higher among people of Black ethnicity.
According to the latest data from the UK Health Security Agency, people of white ethnicity made up the majority of all new diagnoses, but the rate is highest in Black groups when population size is considered.
Here is a graph showing the latest statistics:
But this is far from a new phenomenon - the rate of STI diagnoses has remained disproportionately high in Black men and women since at least 1994.
Research conducted through the Health Protection Research Unit (HPRU) found that there were no clinical or behavioural factors explaining the disproportionately high rates of STI diagnoses among Black people.
But higher rates of poverty and poor health literacy among marginalised communities are all linked with higher STI rates, according to a 2016 study, which found that behavioural and contextual factors are likely to be contributing.
Having sexual partnerships overlapping in time - especially when condoms are not used - is also higher among Black Caribbean people than other ethnic groups, it has been found.
Moreover, experiences of racism among Black people can fuel a reluctance to engage with sexual health services and test frequently, according to HIV activist Susan Cole-Haley.
She told The Independent. “I very much believe that it is linked to socioeconomic disadvantage and racism, often in healthcare settings, which can be a significant barrier for people accessing testing, for instance, and feeling comfortable engaging with care.”

She said it was important to look at “the wider health inequities that Black communities are facing and around sexual health”.
“We need more funding and we need to tackle the racism that people are experiencing in healthcare settings,” she said.
Government spending on contraception and STI testing and treatment fell by almost 17 per cent between 2020 and 2021, according to a report from the Local Government Association. Local authorities cut £1 billion from the UK public health grant over the past decade.
Meanwhile, calls for these disparities to be tackled have routinely fallen on deaf ears due to “gate-keeping”, another expert said.
Dr Annabel Sowemimo, a sexual health doctor and author of Divided: Racism, medicine and why we need to decolonise healthcare told The Independent: “The idea that communities and, particularly, Black Caribbean communities haven’t been flagging this issue for decades is just a false narrative.
“There’s an extensive history of reproductive health campaigning - particularly amongst Black women - saying that there are risks of sexually transmitted infections and HIV and asking for the facilities and the tools to ensure that they can reduce those infections.
“Often this has gone unnoticed by people that provide services and want to provide a one mode fits-all service for these communities.”

She said charities which could address these issues within their own communities often don’t get funding, with favour given to larger organisations “that do not have facilitators or people that understand the needs of the communities”.
“This is the perpetual cycle that we’re in with addressing health inequalities within Black communities,” she said.
Specialists are now calling upon the government to launch tailored public health messaging campaigns and ramp up efforts to counter these disparities across infection rates.
A 2020 study by BMC Public Health suggested a number of interventions among Black communities, particularly Caribbeans, should be developed to address STI risks. These haven’t happened.
Data from HIV Prevention England and the Terrence Higgins Trust show much lower levels of knowledge about HIV pre-exposure prophylaxis (PrEP) in people of Black African origin living in England than there is among white gay and bisexual men, despite them having a much higher prevalence of HIV than people from other ethnic minorities.
But the risks are stark. Just last year, it emerged that Black women are being disproportionately affected by Trichomonas vaginalis (TV), a lesser-known sexually transmitted infection that can increase the risk of contracting HIV if left untreated.

All sexually transmitted infections can be treated but some, such as chlamydia, can harm fertility if it goes undetected and HIV patients, left without care, face lethal risks.
According to Dwayne Wilson-Hunt, chair of the racially minoritised special interest group within the British association of sexual health & HIV (BASHH), healthcare providers aren’t doing enough to support the needs of racially minoritised communities.
“Until very recently, there have been no interventions created to support the needs of racially minoritised communities and that needs to be fixed,” he said.
People are accessing services online, Mr Wilson-Hunt highlighted, describing that as “encouraging”.
“But the reasons for the disparities are multifaceted and, so, will require a very multifaceted approach, looking at how we can improve and support people from minoritised communities in receiving better sexual health care.”
The department of health and social care told The Independent it is taking action to address disparities in sexual health, pointing to various funding packages it’s rolled out.
“We have committed nearly £4 million to deliver a National HIV prevention programme to reduce the impact of HIV and raise awareness of STI prevention strategies among the most affected communities – including Black communities,” a spokesperson said.
“Additionally, our HIV action plan includes measures to improve access to pre-exposure drugs for groups at risk and we have funded 17 projects aiming to improve the sexual and reproductive health of Black communities in England over the past six years.”

The government says it has also provided over £3.4 billion to local authorities through the public health grant. But council leaders recently warned that these services were at “breaking point”.
Dr Hamish Mohammed, consultant epidemiologist at the UK Health Security Agency, said the UKHSA routinely monitors trends in STIs and shares this data with local authorities to help guide local decision-making and to take action to reduce sexual health inequalities.
Dr Habib Naqvi, director of the NHS race and health observatory, said: “Stark variations in access, experience and outcomes, embedded in socio-economic and structural factors, must not be allowed to continue.”



Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments