Breast cancer drug may slow growth of aggressive childhood brain tumour – study
A child with the tumour who was given the drug is now undergoing further treatment, more than four years since diagnosis, researchers said.
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A drug already available on the NHS to treat breast cancer may also slow the growth of a rare and aggressive childhood brain tumour and prolong life, early research has shown.
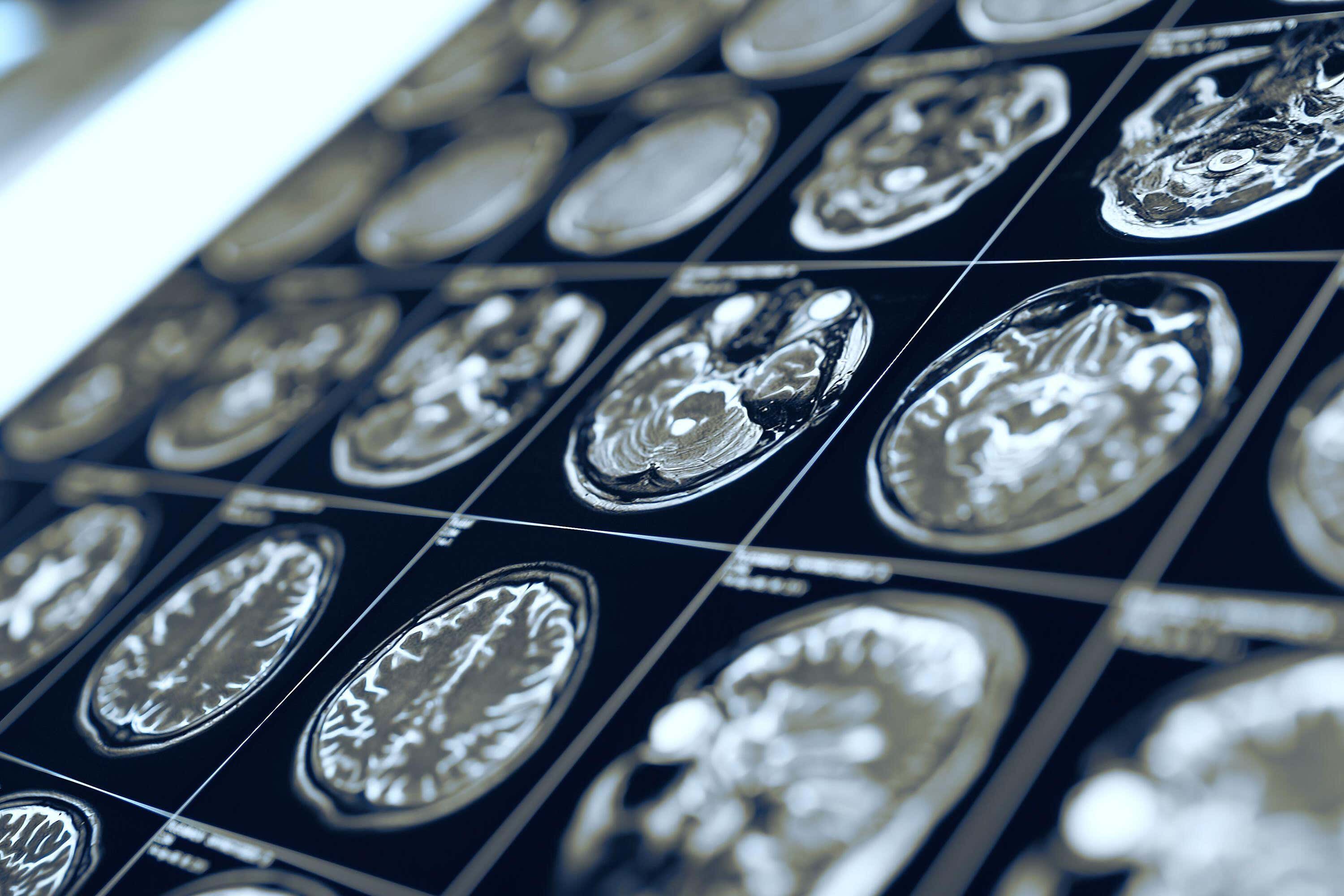
Scientists have found ribociclib, also known by the brand name Kisqali, can keep a subtype of diffuse hemispheric glioma (DHG) stable for around 17 months before it starts to grow back – a disease that would otherwise progress within four months.
A child with the tumour who was given the drug is now undergoing further treatment, more than four years since diagnosis, researchers said.
This is the first time a drug like this has shown promise in this type of DHG
They said these results were “remarkable” because there was currently no cure for DHG and it had a poor prognosis, of 18-22 months.
Chris Jones, professor of childhood brain tumour biology at The Institute of Cancer Research, London, said: “This is the first time a drug like this has shown promise in this type of DHG.”
In the study, partly funded by The Brain Tumour Charity and published in the journal Cancer Cell, the researchers looked at a specific type of DHG that was commonly associated with a mutation in the H3F3A gene.
Lab tests showed that tumour cells disrupted the normal development of nerve cells in the brain.
The team explored whether targeting a protein called CDK6, which is involved in regulating cell division, could prove promising.
Ribociclib is a CDK4/6 inhibitor, which works by shutting down the processes cancer cells need to divide.
As ribociclib can only slow the growth of tumour cells and not kill them, researchers said it may need to be combined with other therapies.
Prof Jones said: “These kinds of drugs have been tested in brain tumours previously with only limited success, so finding one subtype for which they may yet prove useful was a surprise.”
This research helps us have a better understanding of what is driving this devastating disease in children ... Although this is very early days, we hope that it will provide some data to inform clinical trials in the future
While the drug has so far been trialled on one patient, the hope is that the results from this research will lead to clinical trials.
Dr Mariella G Filbin, co-director of the Paediatric Neuro-Oncology Programme at Dana-Farber Cancer Institute in Boston, Massachusetts, US, and senior author on the study, said the results were “unexpected at first, but is now setting the stage for new therapeutic avenues in this disease”.
Dr Simon Newman, chief scientific officer at The Brain Tumour Charity, said: “This research helps us have a better understanding of what is driving this devastating disease in children.
“We know that current treatments are not effective and that finding vulnerabilities in cancer cells could lead to new targeted treatments to help children live longer and better lives.
“Although this is very early days, we hope that it will provide some data to inform clinical trials in the future.”
The research was also part funded by Cancer Research UK and The Billie Butterfly Fund, which was set up in memory of five-year-old Billie Bainbridge who was diagnosed with an incurable brain tumour in June 2011 and died a year later.
Sam Bainbridge, Billie’s dad, said: “We had phenomenal support from friends and family to raise a huge amount of money to help Billie, the money left was donated to The Brain Tumour Charity to fund this important paediatric research.
“We are so amazed to hear that the research has led to positive developments, and while we understand this is not yet the cure we so desperately need, the potential to help children live longer feels like a huge step forward.”
He said he hoped this research “will give hope to families who are now sadly experiencing the horrific circumstances we all endured”.