The Independent's journalism is supported by our readers. When you purchase through links on our site, we may earn commission.
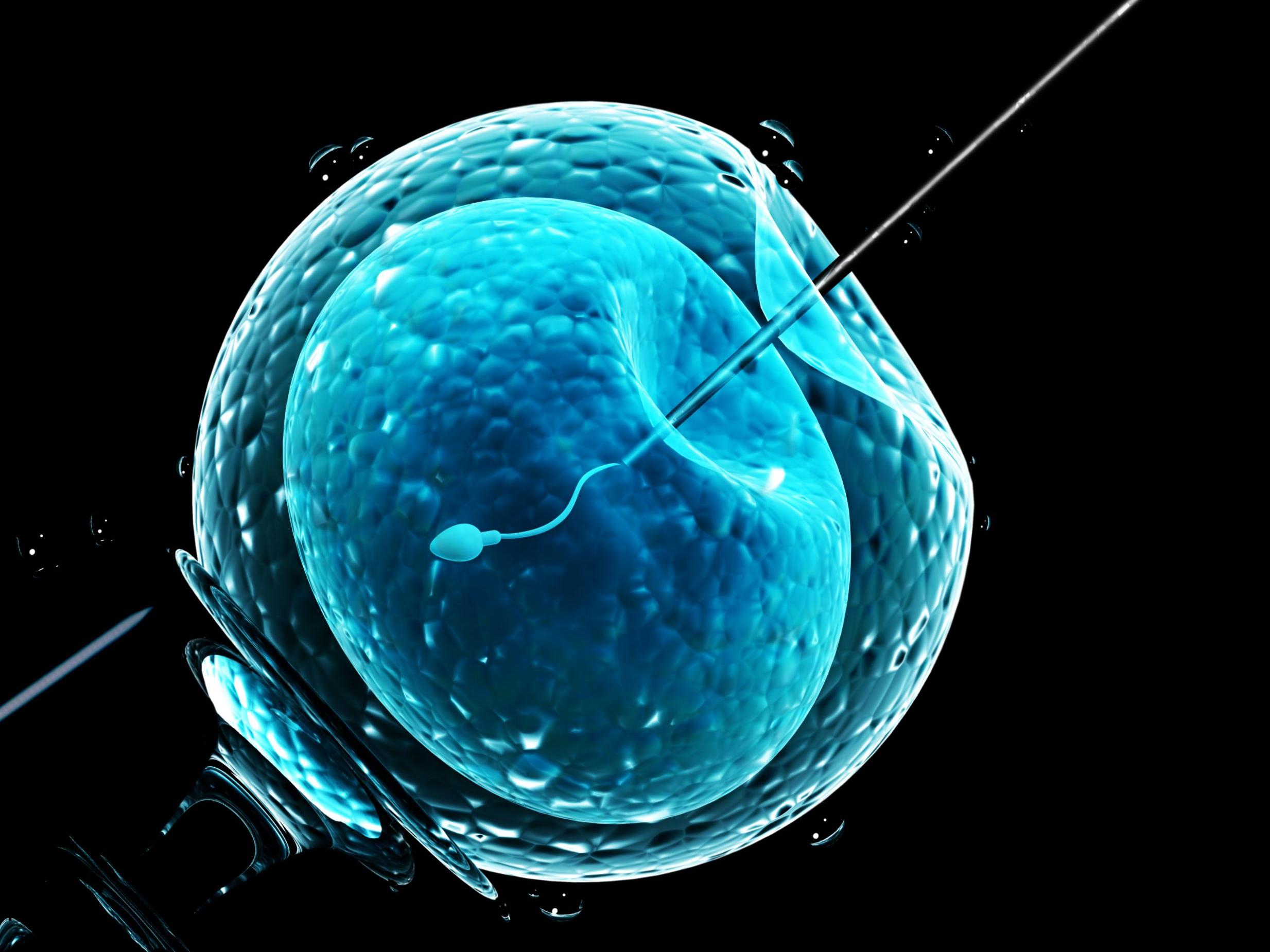
Obese people unfairly denied IVF by cost-cutting NHS, says Oxford academic
‘When organisations like NICE and the NHS get involved by refusing to provide treatments to people on the basis of their obesity, it reinforces this distinction that these people are unable to be helped’
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Obese people are being unfairly denied IVF by NHS bureaucrats who see them as “easy targets” for refusal of the expensive treatment, Oxford University research has concluded.
A paper by health researcher Dr Rebecca Brown said unsubstantiated assumptions that people are overweight by choice, and have become infertile as a consequence of this, result in their applications being declined.
She argues high-quality data from clinical trials – which the NHS demands for other treatments as a matter of course – are scarce or absent for IVF.
What trials there are have shown reduced fertility and pregnancy success rates in people who are obese, but they are less clear-cut on the success rates of the fertility technique.
“There is a lack of evidence about the effectiveness of IVF in anybody,” Dr Brown told The Independent, adding that this was partly because rigorous data-gathering would require some couples to have a placebo treatment.
In England, the National Institute of Health and Care Excellence (Nice) evaluates treatments’ cost-effectiveness. Despite previously saying it would be “illogical” to try to calculate the value of a live birth through IVF, it did produce a report that aimed to do just that and specified that women who are obese, based on their BMI, may not meet this threshold.
However, Dr Brown said it made a number of “rough and ready” assumptions, and gives no consideration to the benefits the male partner might receive from becoming a parent. This methodology “masks other influences, such as negative attitudes towards obese people that render them easy targets for cost-cutting commissioners”, Dr Brown said said in the journal Healthcare Analysis.
Nice does not specify that this means heavier people should be denied IVF. However, the BMI limit is imposed by almost all clinical commissioning groups (CCG) and health boards in the UK – a quarter impose cut-offs on the male partner’s BMI or age.
Sian Gilbert, 29, and her partner have been trying to conceive for six years.
She has polycystic ovary syndrome (PCOS), which means she does not ovulate naturally; this also affects her hormones, making it harder for her to lose weight.
As her partner has fertility issues as well, despite being otherwise healthy, they have been told a more expensive form of IVF known as intracytoplasmic sperm injection (ICSI) is their only chance to conceive.
However, they have never received any form of fertility treatment because of weight BMI restrictions imposed by West Kent CCG.

Ms Gilbert said they have been left “in limbo” since her last meeting with a fertility specialist at Pembury Hospital.
“He literally said, ‘Go away and come back when you’ve lost weight,’” she told The Independent. “That’s it. No advice, no support on how to do that with somebody who suffers from PCOS, nothing.”
While she was regularly playing football and keeping active, an injury has made it harder for her to run or cycle and after recently changing jobs she has struggled to justify the cost of a gym membership.
“With PCOS you kind of get stuck,” Ms Gilbert said. “You’re doing all this work, eating well, doing what you can to lose weight, but it just stops – it’s the most disheartening thing ever.”
Nice told The Independent its guidelines did not specify that NHS organisations should deny IVF to people who are overweight. However, the sustained squeeze on funds means many CCGs use it as a justification to impose ever more restrictive measures.
West Kent CCG has recently run a consultation on lowering the number of IVF cycles it offers from two to one, well below the Nice-recommended three, and although the majority of respondents opposed the cuts it has yet to make a decision.
“When organisations like Nice and the NHS get involved by refusing to provide treatments to people on the basis of their obesity, it reinforces this distinction that these people are unable to be helped by the normal mechanisms,” Dr Brown said.
“If that’s backed up by really good evidence, I don’t think it’s illegitimate to use obesity as a criteria.
“If it’s really dangerous, or completely ineffective, then sure. But that doesn’t seem to be the case, so I speculate that it’s driven by other kinds of things, like an assumption that it’s within people’s control to lose weight and a willingness to treat them less well than we treat other kinds of people.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments