Nurses ‘fear being taken to court’ over degrading treatment of patients in corridors
Staff speak of the psychological toll of working in stretched wards

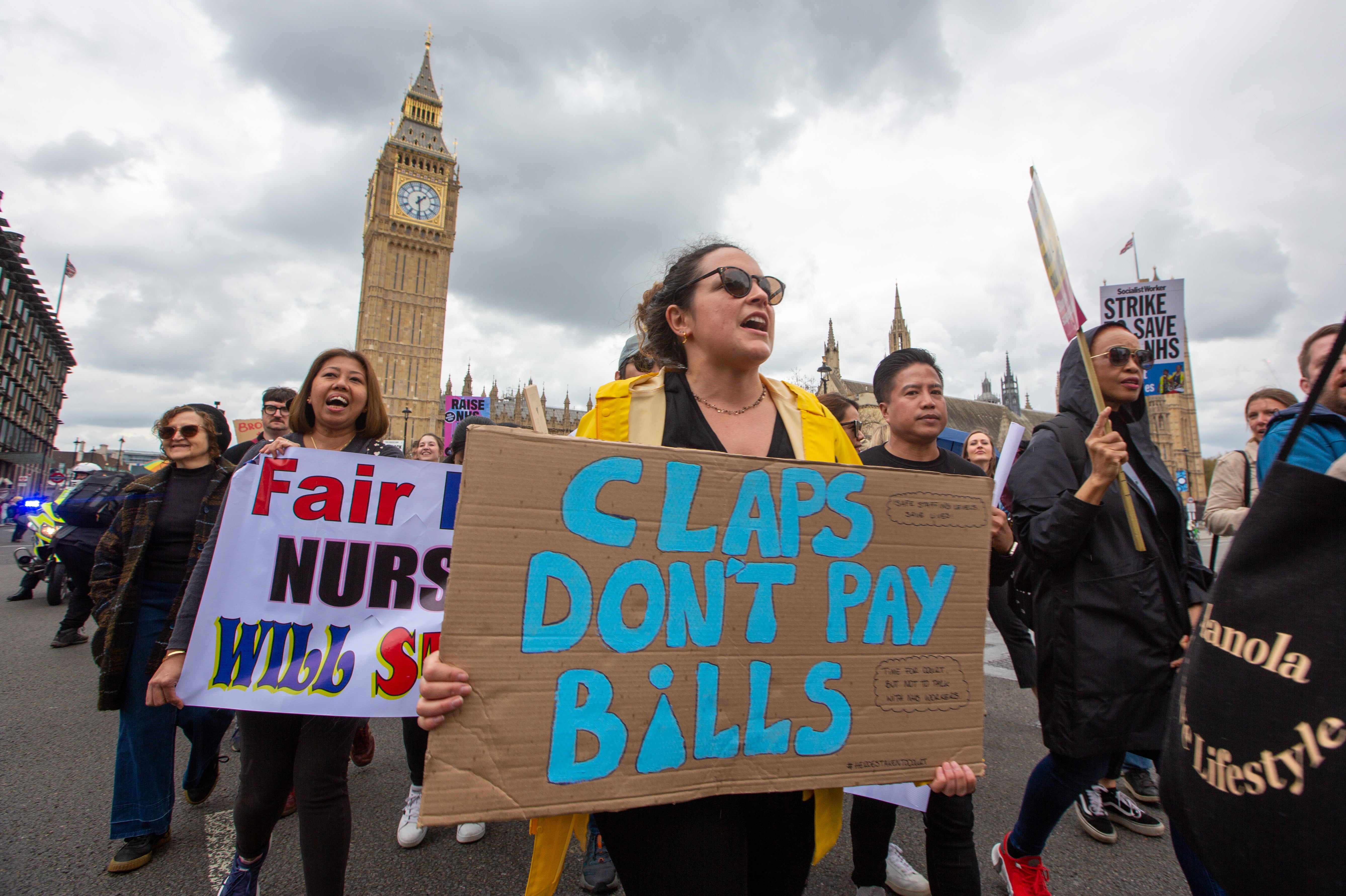
Nurses fear they could be taken to court or struck off over the level of care they are able to give to patients, a union has warned, as the NHS stands on the brink of six more months of strikes.
The Royal College of Nursing, one of the two unions to turn down the recent government pay offer to NHS staff, revealed that over nine in 10 A&E nurses had raised concerns that patients may be receiving unsafe care and that patient dignity, privacy and confidentiality is compromised.
Six in 10 fear they will be struck off the nursing register or have a court case brought against them as a result of patient harm due to their working conditions, the RCN said.
Rishi Sunak has been warned that nurses “are absolutely not going to blink first”, as both they and senior doctors vote on a fresh mandate for nationwide strikes through to Christmas.
Admitting that she herself “may personally have underestimated the members and their sheer determination”, RCN chief Pat Cullen said nurses have shown that health secretary Steve Barclay must restart pay negotiations with a double-digit offer.
Ms Cullen insisted that patient safety is “at the centre of everything that we do” but warned that it “cannot be guaranteed on any day of the week”, given it is missing 47,000 nurses “every single day and night”.
Speaking before its annual congress in Brighton, which begins on Monday, some nurses described themselves as “broken” and feeling “suicidal”, with corridor treatment being deemed “degrading for patients” and as “destroying staff morale”.

One emergency care nurse said: “When you walk into the department and see 15 to 20 people in the queue, day in day out – you lose any hope it’s going to be a good shift.
“We care for patients the best we can, but something happens every day. I’ve dealt with almost every situation I can imagine in the queue. We’ve had to fit call bells and crash buzzers after people have had cardiac arrests in a corridor. Patients who are incontinent need pads changing but there’s no space or privacy to change them.
“Patients and their relatives can sometimes be physically or verbally aggressive towards us because they are rightly scared and horrified about the setting they are being treated in – some are then arrested or removed by security. There are delays to medication. The list goes on.
“Having to care for patients in this way makes you feel you are a terrible nurse. Sadly I have become desensitised to it as I’ve been dealing with it for so long. But unless something is done we will continue to lose brilliant nurses who are getting to breaking point.”
Nurses and doctors find themselves unable to discharge patients due to the lack of community care in place, the RCN says, with bed capacity also deemed to be at a dangerous level.
“This bleak picture comes from right across the NHS,” Ms Cullen said. “Patients backed-up through emergency departments is a stark sign of a health and care system grinding to a halt. A corridor is no place to die and no place to work either.
“When ministers fail to grip this situation, they allow patients to pay a high price and nursing staff to work in fear, professionally compromised,” she said, calling the concerns over legal action “evidence of just how unsafe conditions have become”.
In a fresh blow, senior doctors are also being balloted this week on whether to start striking, with the British Medical Association urging its members to vote for the nationwide six-month mandate, as government talks to resolve their long-running pay dispute remain deadlocked.
A Department of Health and Social Care spokesperson said: “Everyone deserves access to the right care in the right place. That is why we are taking action to cut waiting lists, making it easier for patients to access a GP and have almost reached our target of delivering 26,000 additional primary care staff.
“Our Urgent and Emergency Care Recovery Plan will also mean people are seen quicker as we scale up community teams, expand virtual wards, and put 800 new ambulances on the road.
“We know that if we are to build a stronger NHS it is vital to have the workforce to support it – and their health and wellbeing is of paramount importance. To ease the pressures on healthcare staff, the NHS will soon publish a long-term workforce plan to support and grow the workforce.”
Additional reporting by PA




Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments