Virtual wards and at-home antibiotic kits part of £160m funding to cut NHS waiting lists
Tens of thousands of patients will be part of initiatives including pop-up clinics and one-stop testing facilities
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Virtual wards, at-home antibiotic kits and using artificial intelligence in GP surgeries are among new initiatives to be trialled as part £160m funding to tackle waiting lists in the NHS.
NHS England announced the funding to aid in the health service’s recovery after the pandemic, after figures last month revealed the number of people waiting to begin hospital treatment in England had risen to a new record.
A total of 4.7 million people were waiting to start treatment at the end of February - the highest figure since records began in August 2007.
But NHS England said indicators suggest operations and other elective activity were at four-fifths of pre-pandemic levels in April, which is "well ahead" of the 70 per cent threshold set out in official guidance.
It said it is working to speed up the health service's recovery by trialling new ways of working in 12 areas and five specialist children's hospitals.
The so-called "elective accelerators" will each get some of the £160m as well as extra support for new ways to increase the number of elective operations, NHS England said.
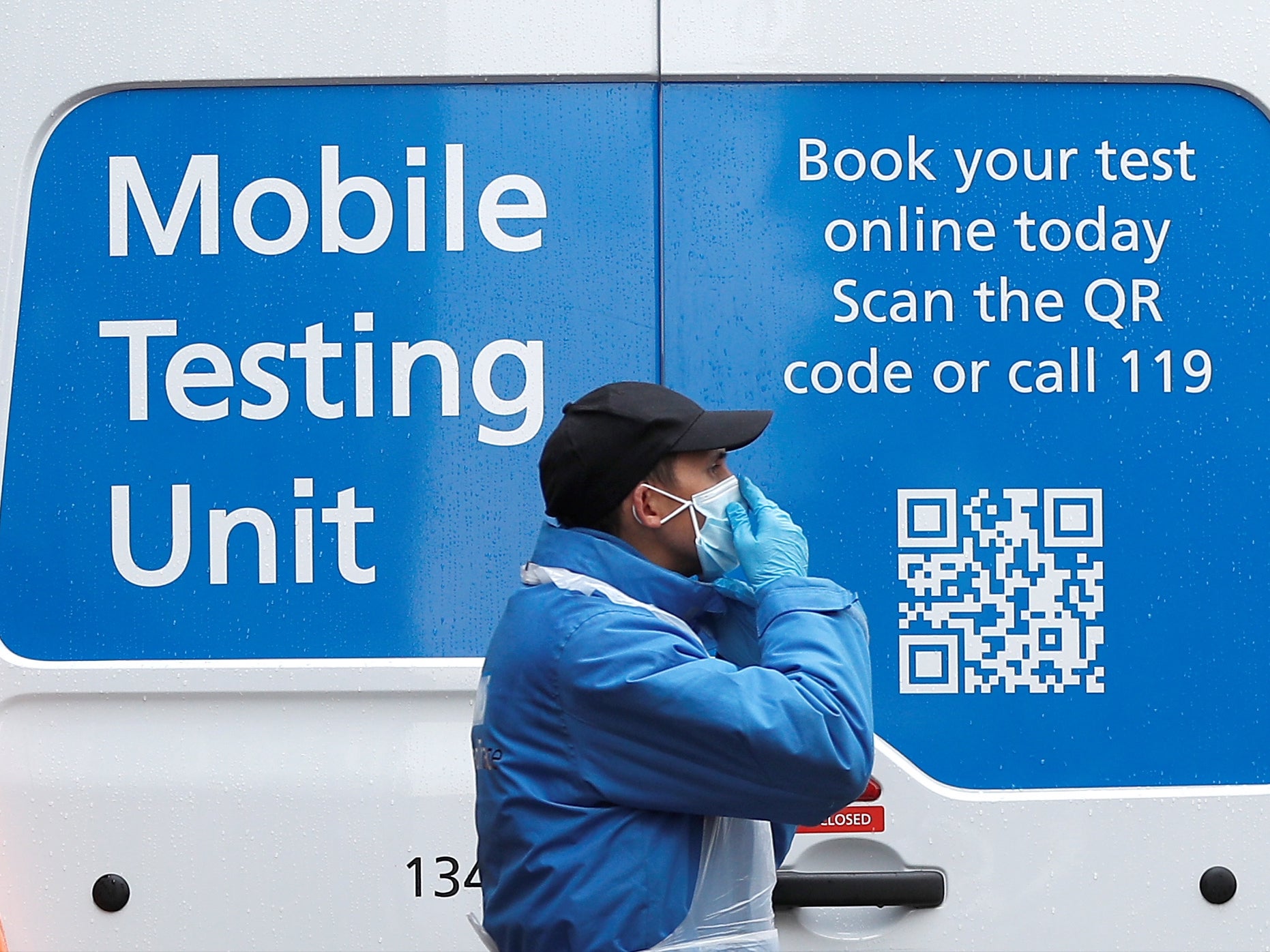
Tens of thousands of patients in the trial areas will be part of initiatives including a high-volume cataract service, one-stop testing facilities and pop-up clinics to allow patients to be seen and discharged closer to home.
Other trials over the next three months include virtual wards and home assessments, 3D eye scanners, at-home antibiotic kits, "pre-hab" for patients ahead of surgery, artificial intelligence in GP surgeries and so-called "Super Saturday" clinics, bringing multi-disciplinary teams together at the weekend to offer more specialist appointments.
Amanda Pritchard, NHS chief operating officer, said: "With Covid cases in hospitals now significantly reducing thanks to the extraordinary success of the NHS vaccination programme, our focus is now on rapidly recovering routine services.
"Early figures show local teams are already well ahead of schedule, but we want to go further, faster, which is why we are investing £160m to find new ways to tackle waiting lists.
"The additional support announced today will help us create a blueprint for continuing that progress over summer and beyond, in a way that doesn't heap extra pressure on staff, so that as many people as possible benefit from the world-class care the NHS provides."
Rachel Power, chief executive of the Patients Association, said lengthy waiting times have been a "worry" for patients and welcomed the initiative.
She said: "The importance of treatment being timely, to ensure the best possible outcomes, is well recognised.
"Effective communication with patients at this critical juncture is also essential, and we have been pleased to work with NHS England on developing principles for effective communication with patients about their elective treatment."
A recent report by the British Medical Association estimated it will cost £4bn to clear the backlog of patients in England in need of elective care, its council chairman Dr Chaand Nagpaul said.
He added: "So to trumpet a cash boost of £160m is wholly disingenuous."
He said the idea of "Super Saturday" clinics showed "a grave lack of understanding of the rocketing workload and demand already facing GPs".
He said: "What we need to see is a workable plan that sufficiently supports the needs of the health service as a whole, and it is imperative that the allocation of funding and resources is reasonable and caters to the needs of primary, secondary and community care - all of whom have been completely stretched in the past year.
"Importantly, this must be underpinned by ongoing efforts to expand the medical workforce and to ensure that the utmost is done to retain doctors and NHS staff and give them enough support through the challenging time ahead."
The chief executive of NHS Providers, Chris Hopson said: “Trusts are working extremely hard to tackle the backlog that was made much worse by the pandemic. They are treating the most urgent cases as fast as they can and are already ahead of the activity targets they were set.
“This is on top of successfully rolling out the vaccination campaign, dealing with demand for urgent care that has now returned to normal levels and very significant increases in demand in areas like children and young people’s eating disorders.
“Trust leaders are telling us that, in the places with the biggest challenge, getting through the backlog could, on current trajectories, take between three to five years. We know this is unacceptable and that the NHS needs to develop a bold, radical, plan to go a lot faster, with appropriate extra funding from the government.
“That’s why this initiative is so important – it will enable a group of pilot trusts to identify a blueprint that every trust can use and adapt to speed up getting through their care backlog.”
Additional reporting by PA
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments