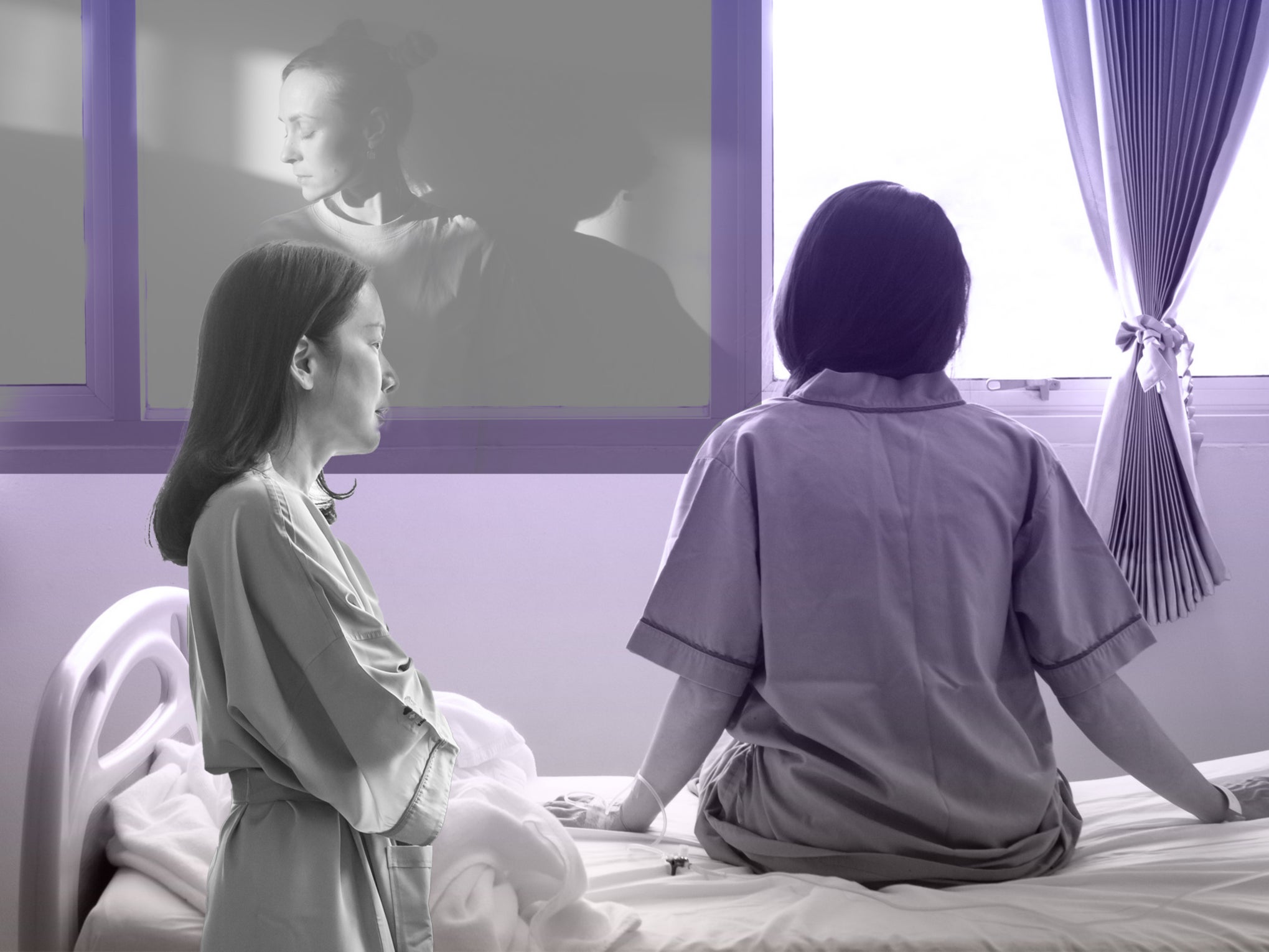
‘My time in a children’s mental health hospital left me with PTSD’
The Independent has spoken to 22 young women who allege awful treatment in private mental health hospital units across a decade from 2012 to 2022. Here some of them recount their experiences

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Young women have told of their “humiliating” experiences at a group of private mental health hospitals over the last decade as part of a joint investigation by The Independent and Sky News.
The Department for Health and Social Care has now launched a probe into the allegations of 22 former patients of units run by The Huntercombe Group, which has run at least six children’s mental health hospitals, between 2012 and this year.
Here, some of those young women recount their experiences:
‘We were treated like animals’
May*, Huntercombe Hospital, Maidenhead; Huntercombe Hospital, Stafford and Watcombe Hall from 2016 to 2018: “They knew little on how to treat someone with eating problems, so I don’t know why I got sent there. So instead of trying to help me, they spent their time drugging me up and force-feeding me. I would get awoken by staff members restraining me out of bed and dragging me down to the de-escalation room to force-feed me.
“I went days without even being allowed in the garden as you have to earn fresh air time. I felt like we were treated like animals. Punished for struggling. I feel like prisoners were treated nicer than us patients.”
‘I was being restrained up to ten times a day’
Amy*, Maidenhead 2021-2022: “I was being restrained up to ten times a day, sometimes for hours at a time, by four or five people...sometimes it was all men...patients were left naked in their rooms under anti-ligature blankets because they wouldn’t buy anti-ligature clothing. Patients would purge in corridors, constantly vomit after feeds and have to stay in their vomit-soaked anti-ligature clothes until they could wash them...Staff would be on 12-hour shifts without a break.”
‘Nightmares were a daily occurrence’
Mother of Sally*, Maidenhead 2018: “Eventually it became obvious to all, that our daughter was deteriorating at Huntercombe, and after a battle to secure a transfer elsewhere, she was moved to a really well-run unit in Brighton. It was only then that we became aware of the full extent of the abusive treatment she had experienced as she was finally able to share with us.
“It was very clear, however, that despite being in recovery from anorexia, her symptoms of trauma were pronounced, eventually leading to a diagnosis of PTSD. Flashbacks and nightmares were a daily occurrence, causing chronic fatigue and dissociative seizures... she was offered inpatient rehab, but was forced to decline it, so severe was her anxiety around hospitals.
‘My stay was a traumatic, lonely and isolating’
Julia*, Stafford, 2020-2022: “Whilst I was there I felt neglected, uncared for and more of an inconvenience than someone that was there to be supported and helped… At one period during my stay there, I believe they overused medication in an attempt to calm me down; in the space of two days, I had been given three injections, even though they made no effort to verbally de-escalate me first.
“On one occasion, a staff member was very forceful when putting me in restraint, and as he went to pull my arm back, broke my wrist. I ended up in a cast for five weeks. He was allowed back onto the ward soon after this incident and did not apologise to me, despite whether it was accidental or not… Overall, my stay here was a traumatic, lonely and isolating year and a half.”
‘The floor was covered in stains’
Helena*, Maidenhead 2017: “The floor was covered in stains, the walls were covered in blood and faeces…As a person who has suffered from trauma, I find it very hard to be alone with males. Despite telling the staff this multiple times, I was left alone, inside my locked room, on numerous occasions with male staff…during a restraint, I had 7 male staff members in my room alone with me pinning me down. I struggled and my arm hit someone. They got more violent and I distinctly remember someone saying ‘if you hit me again, I’ll hit you back ten times harder because there are no cameras in here and you can’t cry to [name of nurse] about it’".
‘I was choking’
Danae Rackcliff, Stafford, 2017-2019: “I was there mainly because of my eating disorder - anorexia. There was no real eating disorder therapy. They claimed to be skilled to deal with eating disorders on the ward but what they meant is they could put a naso-gastric (NG) feed tube down and feed you.

“There was an incident when I was having an NG tube put me under restraint. Sometimes it can go down the wrong hole and it goes down my airway rather than down to my stomach. So I was choking. They thought I was acting and they carried on for a good few minutes until they eventually admitted that it had gone to their airway.”
“If the CQC [Care Quality Commission] was coming in, announced that they would come around and talk to patients and tell us all to be on our best behaviour...They’d say, alright, the CQC is coming tomorrow so you need to be on your best behaviour, I want the unit to look good.”
‘After leaving, I had to learn to live again’
Nima Hunt, Watcombe Hall, 2017: “Over my time at Watcombe Hall, I witnessed and was subjected to countless horrors. Staff were cold, cruel, and humiliated us during our most vulnerable moments. We were treated like we were criminals, as though our presence was offensive or a nuisance. And we were trapped, either because we were sectioned under the mental health act or we had nowhere else to go and no one else to turn to.
“After leaving, I had to learn to live again. Huntercombe had shattered my trust in not only mental health services but in people. The illnesses which had led to my admission in the first place evolved and intensified and I was more vulnerable than I’d ever been.”
‘I screamed’
Kayleigh*, Maidenhead 2019-2020: “As I screamed, a naso-gastric tube was inserted up my nose, but as it did not go in right, I started choking and begged them to stop. I had complied with all my meals so why were they using a tube? They kept forcing it down whilst holding me in place, one on each arm, one on my legs and one on my head.”
‘I find very painful to think about’
Natasha Beauchamp, Maidenhead 2012: “Since leaving the hospital I have been diagnosed with PTSD and been offered trauma therapy for my experiences in hospital… something I find very painful to think about let alone talk about. I was sedated, restrained every day and injected. I was kept away from all other patients and confined to a small area which I couldn’t leave. The staff would drag me from under tables, strip me naked, throw me in the shower and laugh at me. I was stripped of my clothes in front of male staff.”
--
Active Care Group, which took over the remaining Huntercombe Hospitals in December 2021. Dr Sylvia Tang, chief executive of Active Care Group, said most of the alleged incidents date from before its ownership. She added: “Even so, we are very saddened and concerned to hear about these patient experiences as the wellbeing, health and safety of our patients has always been, and continues to be, our top priority. Our clinical teams are led by qualified and compassionate professionals.”
The provider said it delivers its services in line with specifications set out by the Royal College of Psychiatrists and the National Institute of Clinical Excellence and is regulated like other hospitals by the CQC.
The former owners of The Huntercombe Group, now called Eli Investments, said: “We regret that these hospitals and specialist care services, which were owned and independently managed by The Huntercombe Group, failed to meet the expected standards for high-quality care. The Huntercombe Group was sold in March 2021 and the 12 hospitals and specialist care services that were the subject of that sale are now part of the Active Care Group. We wish Active Care Group well in their ongoing operations.”
NHS England said it had “repeatedly” made clear services must provide safe quality care, “irrespective” of whether they are NHS or private.
*Patients have had their names changed to preserve their anonymity

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments