Woman survives cancer against the odds thanks to experimental drug
Doctors hope the medicine may eventually be used for a range of cancers.
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A woman with deadly bile duct cancer is surviving against all the odds thanks to a new experimental drug.
Carol Hardy, 65, is taking part in a clinical trial the Christie NHS Foundation Trust in Manchester, and doctors hope the drug may eventually be used for a range of cancers.
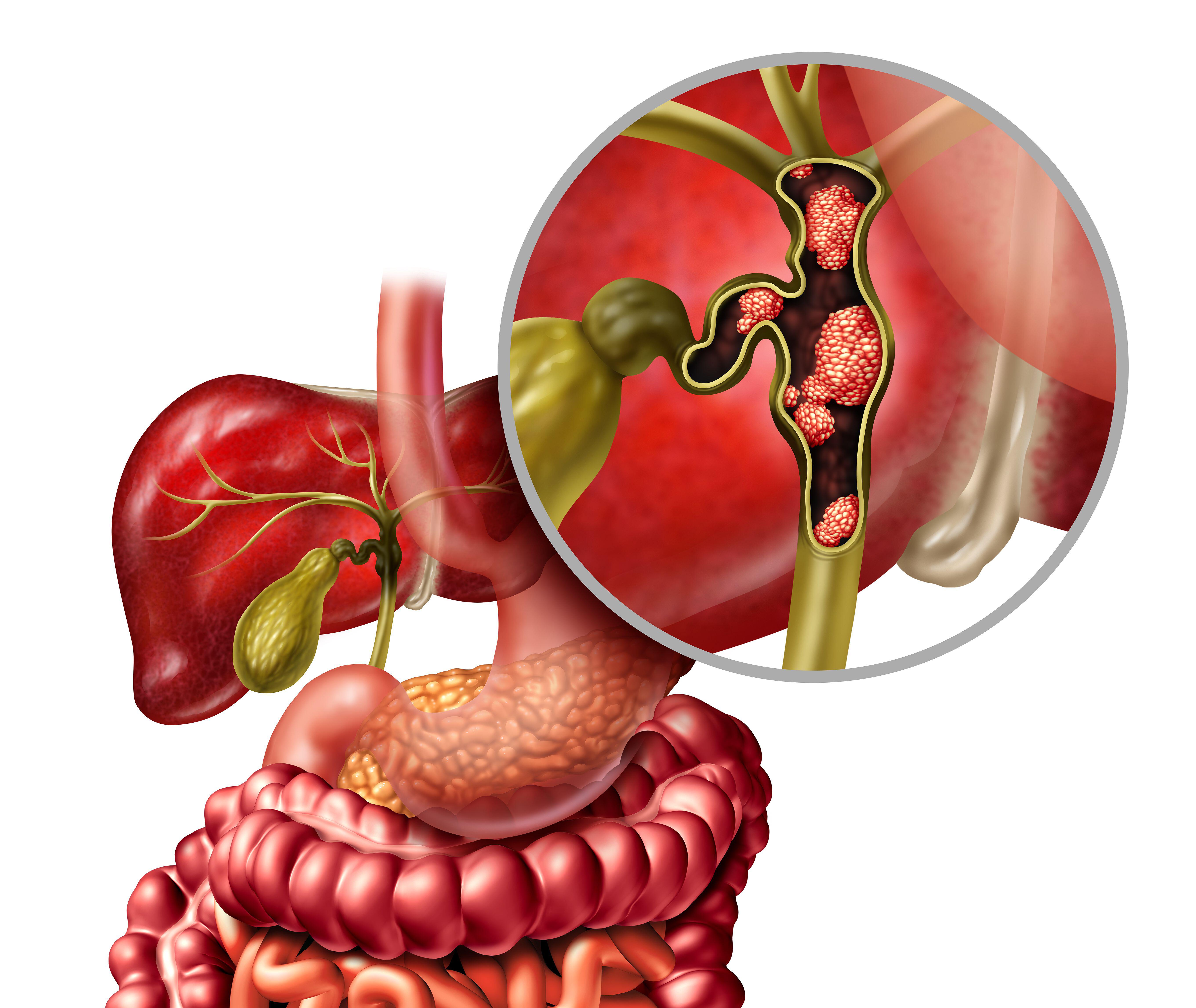
The tablets – known only as RXC004 – contain a compound that blocks a pathway known to be over-activated in bile duct cancer.
So far, the treatment is working and has shrunk Mrs Hardy’s tumour to just over a fifth of its original size.
Bile duct cancer is rare, with around 1,000 new cases every year in the UK.
It does not usually cause symptoms in the early stages but can lead to jaundice, itchy skin, weight loss and pain as it progresses.
Most people with bile duct cancer already have advanced cancer by the time they are diagnosed, with the disease having spread to other parts of the body.
Treatment is usually chemotherapy but only around 5% of people live for five years or more after diagnosis.
Mrs Hardy, from Penrith in Cumbria, discovered she had bile duct cancer by chance about four years ago after suffering gallstones. She had also been losing weight without trying.
She told the PA news agency she had a “sinking feeling” when first diagnosed and was worried about what it meant for her husband Simon, now 55, and daughter Holly, now 22.
My words were 'I can't have cancer, I can't die because my daughter is only 18'
“I can remember being sat on the seat next to my husband,” she explained. “All I can say is, it is as if your chair has been shot back down a dark passage.
“I heard somebody say something, but as the doctor touched my arm and said something to me, I realised it was me that had spoken.
“My words were: ‘I can’t have cancer, I can’t die because my daughter is only 18.'”
During a long operation, Mrs Hardy’s gallbladder was removed and she was given the all-clear from cancer.
But the following year, a scan showed cancer on her liver and in some lymph nodes, confirming that the disease had spread.
If I hadn't got on the trials at the Christie, I wouldn't be alive
Mrs Hardy was referred to the Christie in Manchester and started a trial of immunotherapy combined with chemotherapy.
This shrank her liver tumour down from 2.4cm in September 2020, to 0.9cm in December 2020 and even further to 0.3cm in November 2021.
However, medics found another small tumour on her liver a few months later.
Mrs Hardy was then put on the trial testing RXC004 and has been on the drug since February.
In the most recent scans, Mrs Hardy’s liver tumour has shrunk from 3.3cm in February to 0.7cm now.
She said she has always been determined to fight the disease.
“It’s such shock when you’re diagnosed… but I’ve always been a fighter,” she said.
“To me, in my mind, it was like: ‘right, this is what’s happened, what are you going to do about it? What can you do?’
“And that’s how I dealt with it.
“If I hadn’t got on the trials at the Christie, I wouldn’t be alive.”
What it's doing is actually blocking one of the signal pathways that we know tends to be over-activated in biliary tract cancer
Mrs Hardy is being treated by Professor Juan Valle, a leading expert in biliary tract cancer (which includes bile duct cancer) and member of national and international research groups dedicated to improving treatments for patients with the disease.
He said that about 10 to 15 years ago, there were no trials at all for these rare cancers.
“We saw breast cancer, lung cancer, bowel cancer all developing new treatments, and we couldn’t get out of the starting box with biliary tract cancer because it was thought it was too rare,” he said.
“But in fact, the problem was, there was no collaboration. So, if you put the whole of the UK together, there are enough patients with biliary tract cancer to run proper trials… We can make progress in the field.”
Prof Valle said adding immunotherapy to chemotherapy when patients are first diagnosed has been shown to boost survival.
He said Carol had done well on this combination, but “as happens with most patients, at some point, the cancer started getting worse again.”
At this stage, the trial Carol is on wouldn't change practice, but it would be the springboard to a much bigger trial
This is why he decided to try her on RXC004.
He said: “What it’s doing is actually blocking one of the signal pathways that we know tends to be over-activated in biliary tract cancer.
“Somehow in biliary cancer this is switched on … So what the new compound does is it actually blocks that pathway.
“It’s very early days still. In terms of early drug development, we’re excited by Carol’s story about how well this is doing, but obviously we need to test it in a bigger group of patients.
“At this stage, the trial Carol is on wouldn’t change practice, but it would be the springboard to a much bigger trial.”
The Christie has two groups testing the new drug – Carol and one other patient with biliary tract cancer, and two patients with pancreatic cancer.
Cancer centres across the UK are also recruiting, with the hope 20 patients can be put on the trial.
Prof Valle said tissue samples were needed from patients with rare cancers so they can be molecularly profiled to work out which treatments could help them.
I want to see my daughter grow, get married, perhaps have children if she wants to
“We’re thinking now very much with these patients, not just about the first treatment,” he said.
“We want to have a treatment plan, so that we have a plan A follow by plan B if things get worse and, ideally, a plan C.
“My personal enthusiasm is to enrol patients in clinical trials because, without those trials, we actually make no progress.”
There is a hope that the drug in the clinical trial could be used for other cancers, possibly including bowel cancer.
As for future goals, Mrs Hardy said just wants to spend as much time as she can with her family.
“I want to see my daughter grow, get married, perhaps have children if she wants to,” she said.
“Those are the things that can upset you…. You just want to live as long as you can.”