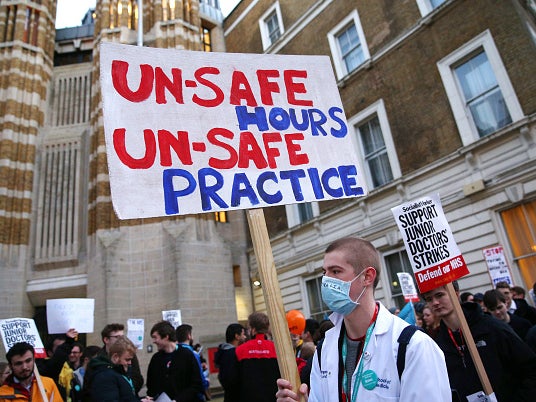
Exhausted junior doctors could increase risk of patient mistakes, report warns
‘A vulnerable person in hospital wants to be cared for by well-rested doctors who are alert and capable of making the best clinical decisions for their patients’
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Patients are being put at risk by “stark” levels of exhaustion among junior doctors, laid bare in the first major survey since a new contract to make the NHS safer at weekends came into force last year.
The General Medical Council (GMC) warned nearly a third of junior doctors say they are exhausted before the work day even begins, according to the results of its annual nationwide survey of medical training.
Safety groups said the findings would be “concerning for patients across the country” as tired doctors are more likely to make mistakes.
They called on those in charge of medical education to act quickly to ensure doctors had time to care for themselves and their patients.
Protection for junior doctors’ training and welfare was meant to be central to the contract pushed through by health secretary Jeremy Hunt in the face of unprecedented strike action in 2016.
It has affected all junior doctors since October last year, and saw “guardians of safe working hours” introduced to offset concerns about the extra weekend and evening working it required.
But the GMC findings on burnout revealed a widespread culture of long and intense hours and heavy workloads, which are “affecting doctors’ training experience and their personal wellbeing”.
The regulator polled almost 52,000 doctors in training and 19,000 of their trainers across the UK.
It found that almost a quarter of trainees (24 per cent) and one in five trainers said they feel burned out because of their work. Many said they were missing training opportunities to cover staffing gaps elsewhere.
Roughly one-third of trainees (32 per cent) said they were often or always exhausted in the morning at the thought of another day at work. Half said they were always worn out by the end of the day.
It also found one in five said that they feel short of sleep at work.
“Patients across the country will be concerned by these findings,” said Rachel Power, chief executive of the Patients Association. “Tired doctors make more mistakes – and patient safety suffers as a result. A vulnerable person in hospital wants to be cared for by well-rested doctors who are alert and capable of making the best clinical decisions for their patients.”
Charlie Massey, chief executive of the GMC, said: “Training must be protected and it must be safe, and employers need to address this urgently. But it is also important that the wider issues reported in our surveys, around work-life balance, burn-out and exhaustion, are acted on.
“We can put off no longer the need to give doctors in training – who make up a fifth of all doctors – the resources they need and deserve.”
The GMC said it is working to ensure doctors were confident that if they raised staffing concerns these would be addressed, but said “it will take investment” to solve these issues.
Theresa May recently announced a £20bn increase in NHS funding over the next five years, but a report by the group NHS Providers warned that nearly all of this would be used up repairing the damage of eight years of austerity.
A Department of Health and Social Care spokesperson said of the GMC figures: “We know how hard our junior doctors work and we are making sure they get the support they need to provide high-quality care for their patients – that’s why we recently announced brand new measures to help staff improve their work/life balance, as well as the biggest ever increase in training places for doctors, including five new medical schools.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments