‘Superhuman’ AI that predicts disease and early death risk to be trialled in NHS
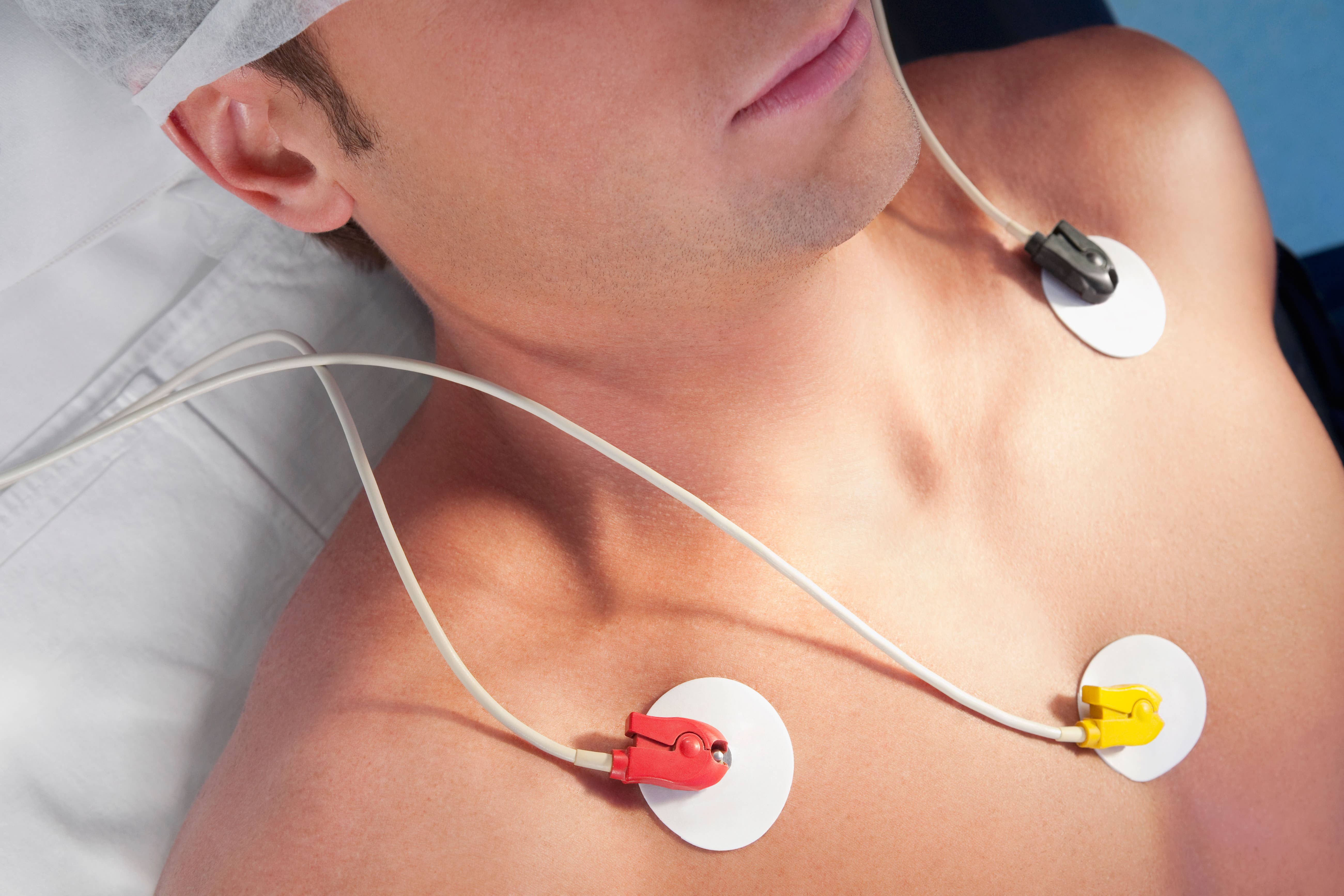
The platform reads the results of electrocardiogram tests, which record the electrical activity of the heart
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A “superhuman” artificial intelligence model designed to predict a patient’s risk of disease and early death is set to be trialled in NHS hospitals next year.
It is hoped the technology – which uses the readings of a common and cheap heart test to alert doctors to patients who may benefit from further tests or treatment – will be used across the health service within five years.
The AI program, known as AI-ECG risk estimation, or Aire, was developed to read the results of electrocardiogram (ECG) tests, which record the electrical activity of the heart and are given to patients suspected of having heart problems.
It then uses these recordings to detect issues in the structure of the heart that doctors would not be able to see.
The technology will be trialled at Imperial College Healthcare NHS Trust and Chelsea and Westminster Hospital NHS Foundation Trust from the middle of 2025, with other hospital sites to be confirmed.
The vision is every ECG that will be done in hospital will be put through the model
Dr Fu Siong Ng, a reader in cardiac electrophysiology at Imperial College London and consultant cardiologist at Imperial College Healthcare NHS Trust, told the PA news agency: “There are three or four different studies that are going to run across hospitals from the middle of next year.
“They are broadly to test that these models are accurate in picking up diagnoses. So, people who would already have an ECG at the hospital, we would test that these models are accurate in picking up certain diagnoses.
“Then the next layer, once that’s been shown, we can intervene to show that we can change the trajectory of the patients.”
It is understood several hundred patients will be recruited for the first trial, with numbers then scaled up for following studies.
Dr Ng added: “The vision is every ECG that will be done in hospital will be put through the model.
“So anyone who has an ECG anywhere in the NHS in 10 years’ time, or five years’ time, would be put through the models and the clinicians will be informed, not just about what the diagnosis is, but a prediction of a whole range of health risks, which means that we can then intervene early and prevent disease.
“If, for example, it says you’re at high risk of a specific heart rhythm problem, you could be more aggressive in preventative treatment to prevent it from happening.
“There are some linked to weight, so you can put them through weight loss programmes.
“You might even think about earlier medical treatments to prevent things from progressing, but that will be the subject of the clinical studies that we plan to do.”
Dr Arunashis Sau, a British Heart Foundation (BHF) clinical research fellow at Imperial College London’s National Heart and Lung Institute and cardiology registrar at Imperial College Healthcare NHS Trust, told PA the aim of the Aire is not to develop something to replace doctors, but to create something “superhuman”.
“The goal here is to try and use the ECG as a way to identify people that are at higher risk, who will then maybe benefit from other tests that could tell us more about what’s going on,” he said.
One key distinction is that the goal here was to do something that was superhuman - so not replace or speed up something that a doctor could do, but to do something that a doctor cannot do from looking at heart tracing
“ECG is a very common and very cheap test, but that could then be used to guide more detailed testing that could then change how we manage patients and potentially reduce the risk of anything bad happening.
“One key distinction is that the goal here was to do something that was superhuman – so not replace or speed up something that a doctor could do, but to do something that a doctor cannot do from looking at heart tracing.”
It comes after research published in Lancet Digital Health found Aire was able to correctly identify a patient’s risk of death in the 10 years following the ECG, from high to low, in 78% of cases.
For the study, the team trained Aire using a dataset of 1.16 million ECG test results from 189,539 patients.
The platform could also predict future heart failure in 79% of cases, future serious heart rhythm problems in 76% of cases, and future atherosclerotic cardiovascular disease – where the arteries narrow, making blood flow difficult – in 70% of cases.
Dr Sau said: “We know that not only doctors, but patients, need to trust AI. And that’s a big part of the work that we did here.
“What we found is that AI could pick up things to do with the patient’s heart structure and function, and even things as deep as genetic information were being picked up that the AI could be using in combination to find out that these people might be at higher risk, and these are things that are not not apparent to human clinicians.”