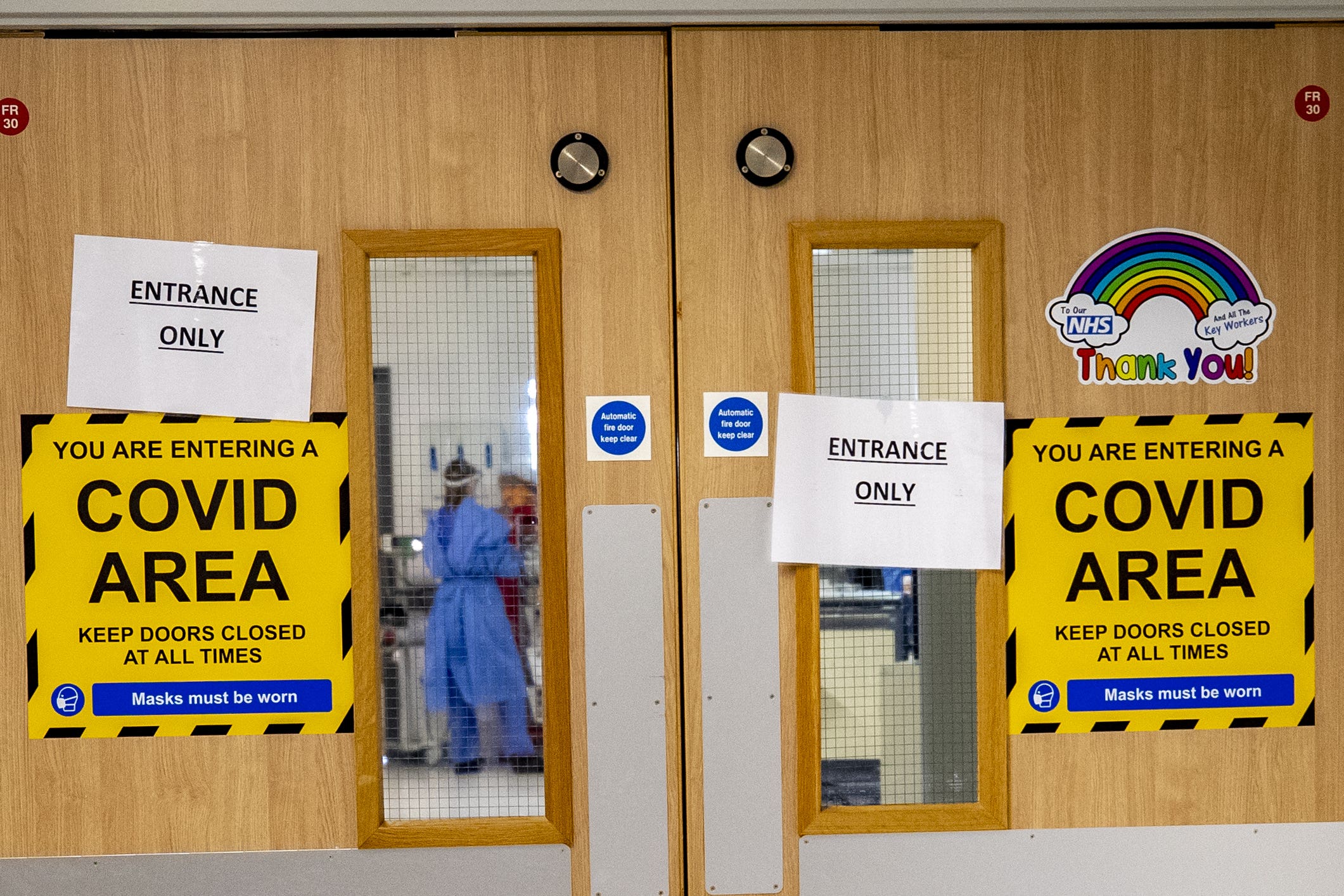
Up to 167,000 people caught Covid in hospital in second wave of pandemic – study
Researchers said the findings revealed the scale of hospital transmissions and highlighted contributing factors.
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.An estimated 95,000 to 167,000 people may have caught coronavirus in hospitals between June 2020 and March 2021, during England’s second wave of the pandemic, a new study suggests.
Researchers say the findings reveal the scale of hospital transmissions and highlight contributing factors, including a limited number of single rooms.
This indicated that hospitals needed to be better equipped to limit the transmission of future viruses.
Hospital transmission of Covid-19 puts vulnerable people at risk, affects healthcare workers and potentially drives transmission in the community.
These findings reveal the previously unrecognised scale of hospital transmission
But there has been little work to assess the extent of hospital transmissions.
Ben Cooper, from the University of Oxford, and colleagues tried to address this knowledge gap by assessing data from 145 English NHS acute hospital trusts, including 356 hospitals with a combined bed capacity of approximately 100,000.
Data included incidence of Covid infection, staff absences due to the virus and classification of the likely source of infection.
Prof Cooper, said: “This study represents the first data-driven attempt to understand the drivers of Sars-CoV-2 transmission in hospitals at a national level and informed efforts to control the hospital spread of Sars-CoV-2 at the time.
“The findings also point to ways we might be able to reduce hospital-based transmission in future outbreaks of other pathogens.”
The study found that between June 10 2020 and February 17 2021, a total of 16,950 and 19,355 Covid infections in hospital patients were classified as having either definite or probable healthcare-associated infections respectively.
The definitions used to classify hospital-acquired infections may only capture around 26% of such infections (for example, many patients may be discharged before testing positive), the researchers estimate.
To that end, they combined reported infection numbers with estimates of the proportion of infections not captured by the classification system in use during the study period.
This resulted in estimates of hospital-acquired infections that range from 95,000 to 167,000.
This would mean that 1% to 2% of all hospital admissions resulted in such an infection over the study period.
According to the findings, there was considerable variation in the rate of hospital-association infections.
The study indicates that the highest rates were seen in the north-west regions of England, and the lowest in the south-west and London regions.
These findings ... have direct implications for targeting of hospital control measures and highlight the need to design hospitals better equipped to limit the transmission of future high-consequence pathogens
The low availability of single rooms and reduced heating of hospital buildings could be factors associated with increased rates of transmission, the research suggests.
The vaccination of healthcare workers was associated with lower infection rates, the study also found.
The authors say that considering these findings could inform measures to reduce hospital transmissions, which could protect vulnerable patients and healthcare workers as well as reduce community transmission.
The researchers say: “These findings reveal the previously unrecognised scale of hospital transmission, have direct implications for targeting of hospital control measures and highlight the need to design hospitals better equipped to limit the transmission of future high-consequence pathogens.”
An NHS spokesperson said: “While hospital infections inevitably rose over the peak of the pandemic’s second wave, the ONS and other data have conclusively demonstrated that the root cause of rising infection rates in hospitals was the rising rates in the community.
“NHS staff followed UKHSA Covid-19 infection prevention control guidance as cases increased to keep patients and staff as safe as possible.”