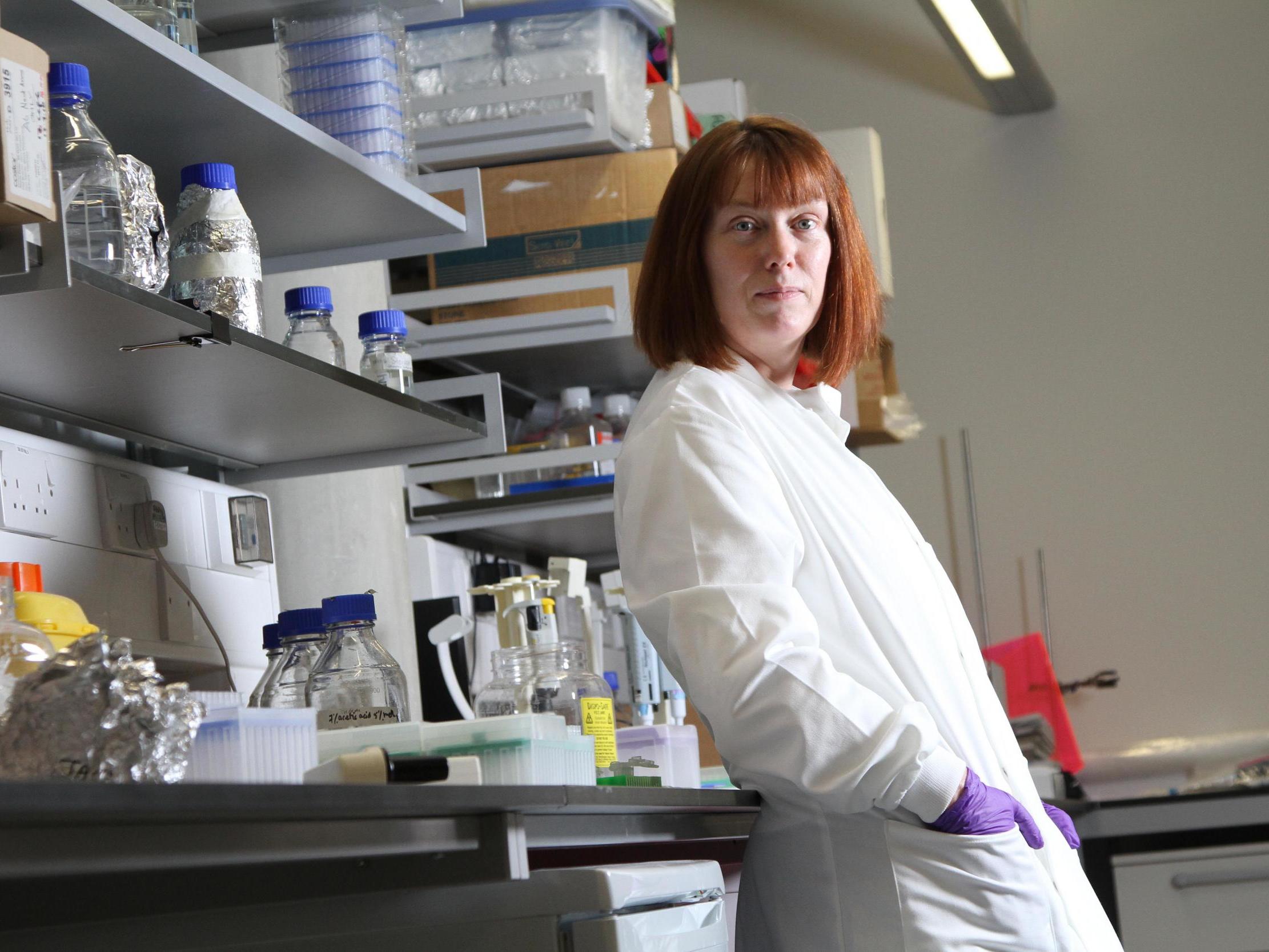
‘You just get on with it’: The Oxford professor carrying the world’s hopes of a coronavirus vaccine
Sarah Gilbert tells Samuel Lovett how decades of experience (and raising triplets) helped her prepare for the challenge of a lifetime

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.More than seven months have now passed since Sarah Gilbert embarked upon the arduous journey of developing a vaccine that will, hopefully, help guide humanity out of this pandemic.
It’s a responsibility that the professor of vaccinology and her team at Oxford University have quietly shouldered, sealed away from the chaos and confusion that has knocked the world off balance, patiently and diligently attending to the task at hand.
With the stakes so high, there has been no scope for respite or distraction. “If it’s not necessary, it gets cut out,” says Gilbert. “When you’re in the situation that you need to do things which could potentially have a large impact, you just get on with it.”
She speaks from experience, both as a leading vaccinologist with a 25-year-long career in developing vaccines against influenza and emerging viral pathogens, and as a mother of triplets. Indeed, as relentless and consuming and sleep-deprived as this year has been, it’s territory she knows well.
“I’m trained for it – I’m the mother of triplets,” says the 58-year-old, adding that all her children are now enrolled in university. “If you get four hours a night with triplets, you’re doing very well. I’ve been through this.”
Still, the emergence of Sars-Cov-2 – the virus responsible for Covid-19 – has brought with it new challenges, new questions, new mysteries for Gilbert and her colleagues to unravel. Like many others in her profession at the moment, she has found herself flung to the forefront of a new frontier.
There has never been a human vaccine developed against any member of the coronavirus family. Gilbert points out that there are two equivalent veterinary vaccines – one bovine, the other avian – but there is no denying the unprecedented nature of the challenge she faces.
Yet, she says, there “haven’t been any doubts over what it is we’re trying to do”. Since the team at Oxford University’s Jenner Institute first jumped into action, there have been few moments that threatened derailment.
Admittedly, there have been “technical hurdles, definitely”. On one occasion, when attempting to produce a second batch of the vaccine at Oxford’s manufacturing facility using a new purifying process, “things just went wrong”. Fortunately, a contract with a manufacturer in Italy, which was already making another batch, meant it wasn’t the end of the road.
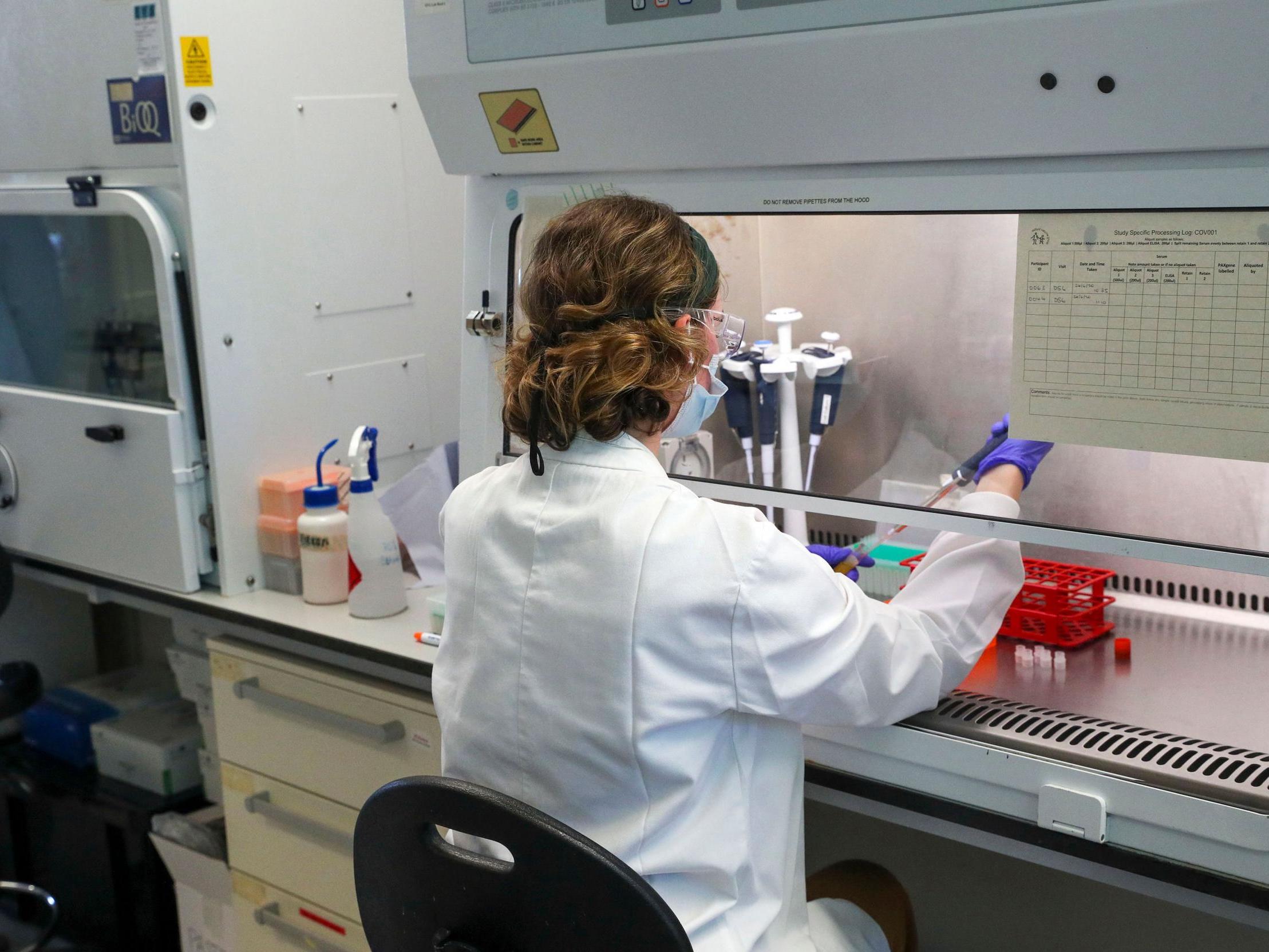
But having moved as seamlessly as possible from preclinical trials to phase one, to phase two and now phase three – which measures the vaccine’s effectiveness in limiting community transmission – Gilbert’s team remains on course to deliver her vaccine, called AZD1222, by the end of the year. AstraZeneca, who has partnered with Oxford to manufacture the candidate, has meanwhile begun producing doses, with a commitment to making two billion by next summer. “Things are going very well on the scale-up front,” Gilbert says.
Questions have naturally been asked of the speed at which Gilbert and other vaccinologists have been moving. Typically, it can take years for a vaccine to be developed, tested and approved. Yet such processes have been condensed into a matter of months, with one of Gilbert’s colleagues announcing this week that Oxford could place its trial data before regulators by the end of the year.
Gilbert insists, though, that no corners have been cut and that should the vaccine gain approval, it will have gone through all the necessary checks and balances. “We’ve been able to find ways to save time when going through all the normal processes,” she says. “We’ve worked with the regulators and ethical committee to minimise the time it takes to get to approval, but the approval is still the full approval – it’s not missing anything.”

She points to “accelerated procedures” that have helped to cut away unnecessary waiting time. “Normally we can’t mention the trial and ask anyone to consider taking part until it’s all completely approved,” she says. “This time we were allowed to advertise the trials and contact people.” Individuals who expressed an interest were then vetted and prepared for vaccination, which only followed once approval was secured. “So we had a cohort of people ready to vaccinate. That doesn’t normally happen.”
Gilbert also explains that, crucially, her team was well prepared for this moment, long before Covid-19 surfaced. Prior to the pandemic, her lab had developed technology to create vaccines against virulent viruses. This approach used a genetically engineered chimpanzee adenovirus — which causes the common flu in apes – to carry elements of a harmful virus into humans, triggering the necessary immune response.
Her work covered the likes of Nipah, Lassa and Rift Valley fever, and, perhaps most significantly, Middle East Respiratory Syndrome – a lethal disease caused by another coronavirus. The framework, she says, was in place for team to hit the ground running with Sars-Cov-2.
“When I started seeing reports of an outbreak in China at the beginning of the year, I saw that and thought, ‘Is that going to be something we should be making a vaccine for?’ I was thinking in terms of our technology.
“There’s a lot that has been done to plan before this year to be able to make a pandemic vaccine quickly, and there’s a lot of research that has been done which we’re now able to take advantage of. Because we’ve been preparing for such a long time, that’s why we can go quickly.”
But not wanting to get too ahead of herself, Gilbert humbly insists “this wasn’t as fast as we could go”, adding: “We didn’t have all the preparations in place. This wasn’t optimised. But we did the best we could.”
One issue that could, in theory, disrupt efforts to vaccinate the human population is the emergence of new mutations in Sars-CoV-2. In the recent case of the Hong Kong man who tested positive for a second time, scientists showed that he had been infected with two different strains of the pathogen. Closer analysis found 24 differences between the first and second viral genome.
There was nothing to suggest that the new iteration of the virus was more aggressive or contagious – if anything, emerging data suggests that the pathogen is becoming less deadly – but it’s impossible to tell how future versions will interact with the human body.
Nonetheless, Gilbert is confident that Sars-CoV-2 won’t evolve to the point of rendering her vaccine redundant. “The mutations arise at quite a low rate in coronaviruses,” she says. “With all the mutations that have been found so far, there’s no indication the neutralising antibodies don’t neutralise them.
“I don’t think that within the coming year we’ll see the virus mutate to the extent the vaccines won’t work. It may be that over two or three years it mutates, so that it’s somewhat reduced efficacy, and then we might decide changing the sequencing in the vaccine will be a good thing.”
This level of optimism doesn’t quite stretch to the longevity of the immune response triggered by AZD1222. Although preliminary trial results have shown that the vaccine trains the immune system to produce antibodies and white blood cells capable of fighting the virus, there is a fear that this protection could fade in time, allowing Sars-CoV-2 to recirculate among populations.
Similarly, it is currently unknown if the threshold for reaching immunity will be passed, as there is no standardised measurement – something that is known as an assay – to draw comparisons with.
“We don’t know what level of immune response we need to protect anybody in the first place. Nobody does,” Gilbert says. “What’s lagging behind is the development of the assays.
“Normally you would have standardised assays before you started phase three trials, so we can measure immune responses, but we’re not sure what we’re measuring.
“If one vaccine is shown to be effective, all of the vaccine developers will want to compare the immune response they get with their vaccine and see if it’s the same, greater or less than that. But we don’t have the assays to be able to compare and to give us this information at this stage.
“Once we know the protection threshold level, we can then follow the immune response taking blood samples and see how long it takes for the antibodies to fall below that level of response.”
For now, Gilbert continues to keep a watchful eye over the progress of the phase three trials – which are being conducted in the UK, US, Brazil and South Africa – while leading ongoing research in Oxford. The next big decision she and her colleagues must make is when, as they say in the business, to “unblind the trial”.
At this stage, Oxford’s statisticians will be counting up the number of participants who have tested positive for Covid-19. Once the researchers believe they have enough cases, it will be revealed which of these individuals were injected with the vaccine and which were injected with a meningitis jab. The process of finding out the efficacy of the vaccine is therefore faster when the transmission is higher in the community.
“The more cases that you get before you look, the more certain you’ll then be of how exactly how effective the vaccine is, whether it’s low or high,” says Gilbert. “You go from being able to say ‘Yes, it seems to be doing something but we’re not really sure how much’, to being very precise about the vaccine efficacy and say that it’s 70 per cent, for example. But you’re not allowed to keep looking, those are the rules.”
The timing of the unblinding feels like, in many ways, somewhat of a gamble, especially with so much riding on this. Although time is of the essence, in shooting their shot too soon, there’s a chance the regulators might not be happy with the results, says Gilbert. “It’s a hard decision to make. It’s not one that has been made yet for our trial,” she adds. “There’s a pay-off between knowing early that it is or isn’t working, and then having greater confidence in the actual level of efficacy.”
Despite her efforts to manage expectations, confidence in the vaccine – whether rightly or wrongly – is running high. On Thursday, the European Commission made a €336m (£300m) down payment to secure at least 300 million doses of the vaccine, joining the likes of the US, Germany and India in placing advance orders.
Gilbert herself is confident that her vaccine, along with many of the other key candidates in development, will ultimately prove effective. “From first principles there’s a very good possibility that we will have multiple vaccines against the coronavirus,” she says. If Oxford’s does the job, “other vaccines will also work”.
The legacy of this pandemic is no doubt set to run deep, altering the very fabric of our society for years to come. Lessons have been learnt – or not, in the case of some countries – and humanity reminded of its fragility in the face of nature. But, as Gilbert says, there’s always more work to be done, more progress to be made in this space.
“I hope it’s much more apparent now to people at large that it’s worth investing in vaccines,” she says. “It’s been difficult to get the investment to make new vaccines against outbreak pathogens because there’s always something else to spend the money on. But now we’ve seen the devastating effect that a virus can have, I’m hoping that we’ll be able to address the balance.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments