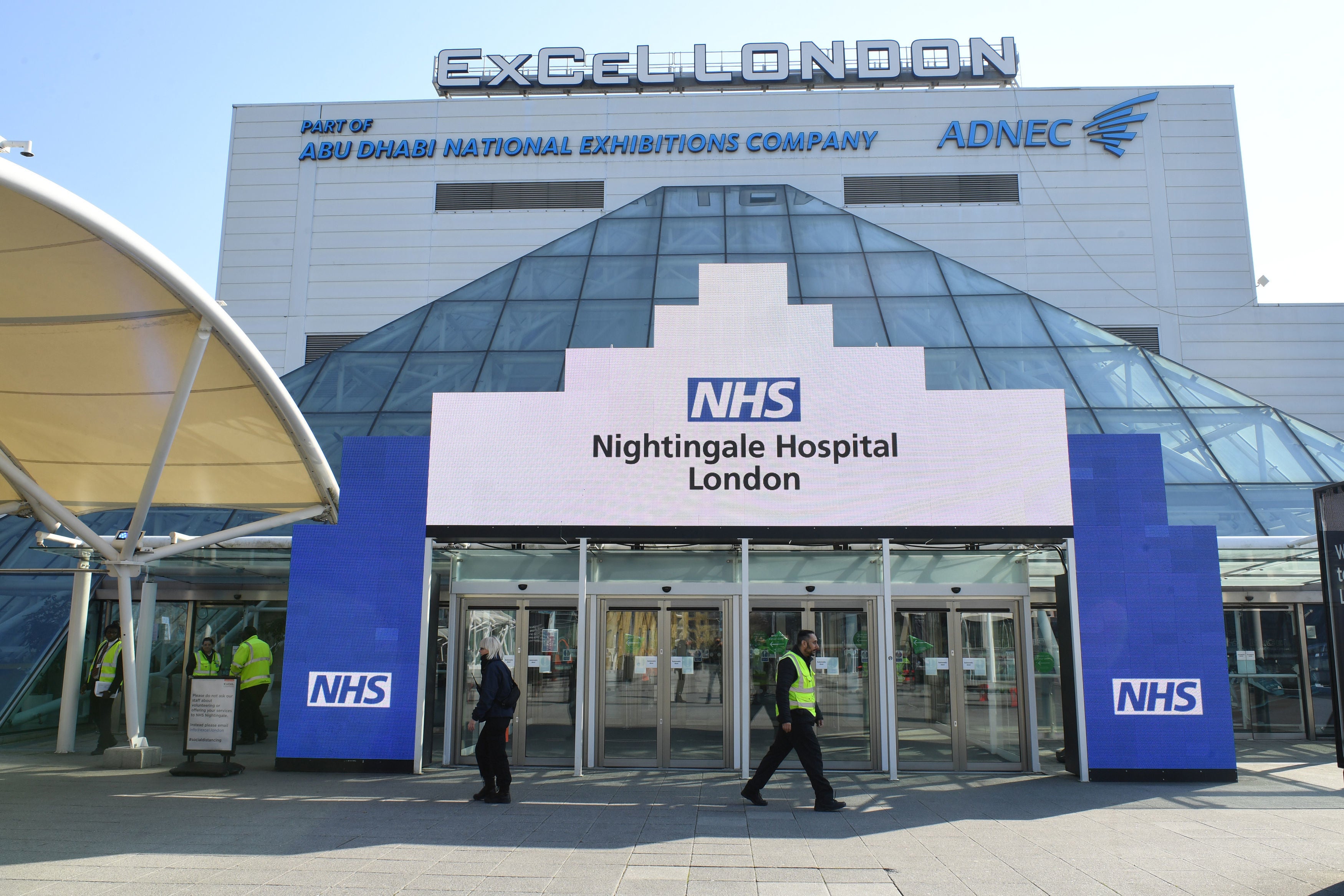
NHS told to prepare for use of Nightingale hospitals in coming weeks
NHS Providers chief warns hospitals are about to face their ‘most difficult and demanding period in the history of the health service’
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.NHS England has told trusts to begin planning for the use of Nightingale hospitals as the number of coronavirus patients is expected to surge in the coming weeks.
In a letter sent on Wednesday night, hospitals were told to activate all of their emergency capacity to cope with the expected pressures.
This is likely to mean the mass redeployment of staff and the designation of wards, surgical theatres and recovery areas as makeshift intensive care units for patients.
NHS England did not explain how the Nightingale hospitals would be staffed if the decision was made to activate them.
During the first wave, hospitals were reluctant to release enough staff to safely run the seven field hospitals around England. As a result, they were barely used with the London Excel hospital, which had space for 4,000 patients, treating only 54. The Nightingales cost £220m to set up.
Saffron Cordery, the deputy chief executive of NHS Providers, said: “Staffing is, of course, the big challenge here. We have a finite pool of staff across the health service – both NHS and private sector. So while we can create the physical capacity to manage high demand, matching that with staff is less easy.”
She said staff had been “incredibly flexible” and were redeployed from lower demand areas to support those who were under greater pressure during previous waves.
“And services – such as outpatient consultations – have been changed and often delivered remotely which can free up key staff,” she added.
“First time round routine care was suspended, which helped. This time we are seeking to manage the backlog of treatments and procedures. This is a balancing act and requires sophisticated judgement calls about when it is right and safe to carry on with routine work and when to focus on Covid and emergency care.”
NHS England has also instructed trusts to discharge as many patients as they can by using all available spare beds in local hospices and sending patients to designated care homes who can isolate them to protect against infection.
Hospitals have been encouraged to adopt a “home first” approach with patients assessed by community services in their own homes.
The NHS in England has reported increasing numbers of patients in hospitals. The latest data suggests the total number of patients is just a 1,000 less than the 18,974 peak set on 12 April.
Many hospitals in the southeast and London have already declared major incidents and cancelled operations in an effort to free up beds. And many hospitals in the north of England still have high numbers of Covid patients as a result of the second wave.
In her letter, Amanda Pritchard, NHS England’s chief operating officer, said: “With Covid-19 inpatient numbers rising in almost all parts of the country, and the new risk presented by the variant strain of the virus, you should continue to plan on the basis that we will remain in a level four incident for at least the rest of this financial year and NHS trusts should continue to safely mobilise all of their available surge capacity over the coming weeks.
“This should include maximising use of the independent sector, providing mutual aid, making use of specialist hospitals and hubs to protect urgent cancer and elective activity and planning for use of funded additional facilities such as the Nightingale hospitals.”
She added that “timely and safe discharge should be prioritised” and urged bosses to do what they can to help the workforce, saying: “Support for staff over this period will need to remain at the heart of our response, particularly as flexible redeployment may again be required.”
Despite the rising pressures on hospitals, NHS England said they should continue to treat as many routine patients as possible and restore services “as close to previous levels as possible” and prioritise “those who have been waiting the longest, whilst maintaining cancer and urgent treatments”.
Ms Pritchard added: “This year has arguably been the most challenging in the NHS’s 72-year history. But even in these most testing times, people across the service have responded with passion, resilience and flexibility to deal with not only the virus but also the needs of patients without Covid-19. The rollout of the vaccine will bring hope to 2021 and we will need to maintain the energy and effort to meet the needs of all we serve throughout the year.”
The latest data for the NHS showed at least 162,000 patients had waited more than a year for treatment in October, a huge rise from February when the number was just 1,163.
The total NHS waiting list has now reached more than 4.5 million, with more than a third of patients waiting more than the 18-week target.
Ms Cordery said: “This letter lays bare the size of the challenges trusts face in what is likely to be the most difficult and demanding period in the history of the health service in terms of managing the pandemic, the task of maintaining and recovering wider NHS services and delivering a large-scale vaccination programme.
She added: “Trust leaders tell us in the face of the pandemic, with consequent pressures on space and staffing, bed occupancy at 85 per cent feels like 95 per cent, and we are currently running at 88 per cent so that is posing real problems.”



Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments