The Independent's journalism is supported by our readers. When you purchase through links on our site, we may earn commission.
Dostarlimab: How does promising cancer drug work?
‘This is the first time this has happened’: All 12 patients involved in US study entered remission after taking dostarlimab over a six-month period
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Scientists have reacted with excitement – and a typical splash of caution – to the news that every single cancer patient in a small clinical trial conducted in the US was cured after being treated with an experimental drug.
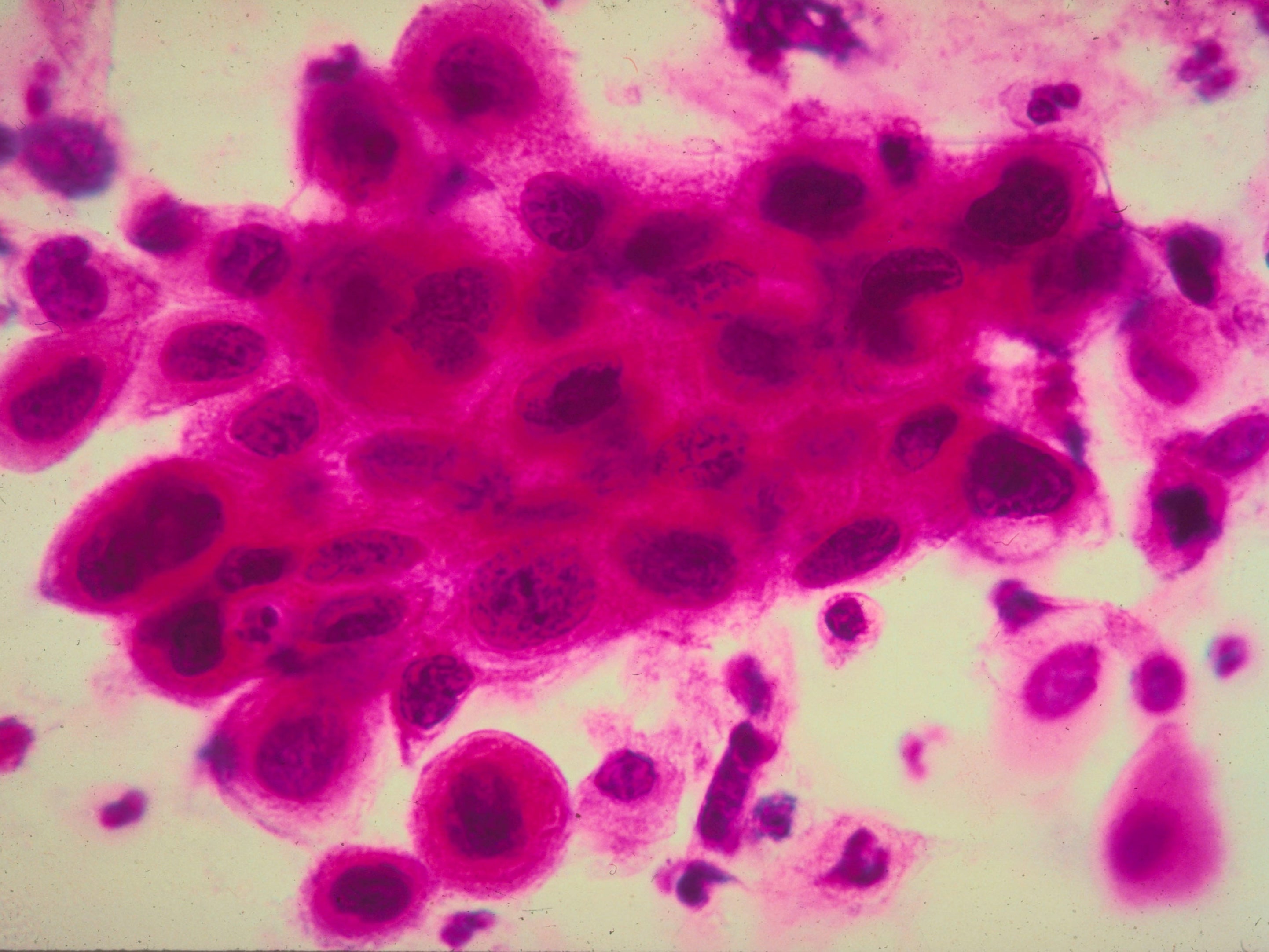
The 12 patients, all of whom had been diagnosed with rectal cancer, entered remission after taking dostarlimab over a six-month period, according to a study published in The New England Journal of Medicine.
The study is, clearly, very small – and scientists have said the results will need to be repeated. But to have 100 per cent remission across all patients is unprecedented and cause for great optimism.
“This is the first time this has happened in the history of cancer,” Dr Luis Diaz, one of the lead authors of the paper and an oncologist at the Memorial Sloan Kettering Cancer Centre in New York, told The New York Times.
So, what do we know about dostarlimab?
It is an immunotherapy drug used in the treatment of endometrial cancer, which affects the lining of the uterus and is highly curable.
The medication, which is administered via intravenous, was first approved for use in the US and Europe in April 2021.
Although none of the patients in the US trial developed clinically significant complications, adverse reactions to dostarlimab typically include fatigue, nausea, diarrhoea and constipation.
The study is the first of its kind to investigate whether dostarlimab can be effective against rectal cancer tumours. Patients received the medication every weeks over a six-month period.
How does the medication work?
Dostarlimab is a checkpoint inhibitor, which works not by directly attacking the cancer itself, but driving a person’s immune system to essentially do the work.
These type of immunotherapy drugs do so by blocking proteins that stop the immune system from attacking cancerous cells.
T cells, which typically seek out and destroy cells infected with foreign pathogens, have proteins on them that turn on an immune response and other proteins that turn it off. These are called checkpoint proteins.
Some checkpoint proteins help tell T cells to become active, for example when an infection is present. But if T cells are active for too long, or react to things they shouldn’t, they can start to destroy healthy cells and tissues. So other checkpoints help tell T cells to switch off.
Some cancer cells make high levels of proteins. These can switch off T cells, when they should really be attacking the cancer cells. So the cancer cells are pushing a stop button on the immune system. And the T cells can no longer recognise and kill cancer cells.
Drugs that block checkpoint proteins are therefore called checkpoint inhibitors. They stop the proteins on the cancer cells from pushing the stop button. This turns the immune system back on and the T cells are able to find and attack the cancer cells.
On average, one in five patients have some sort of adverse reaction to checkpoint inhibitors. While most reactions are easily managed, as many as 3 percent to 5 per cent of patients on the medication have more severe complications that, in some cases, result in muscle weakness and difficulty swallowing and chewing.
Anything else I should know?
All of the 12 patients in the study had tumours with a genetic mutation known as mismatch repair deficiency (MMRd), which is seen in a subset of approximately 5 to 10 per cent of patients with rectal cancer.
Patients with such tumours tend to be less responsive to chemotherapy and radiation treatments, which increases the need for surgical removal of their tumours.
However, MMRd mutations can also make cancer cells more vulnerable to the body’s immune response, especially when it’s bolstered by an immunotherapy agent – in this case, dostarlimab.
What do the scientists say?
Dr Hanna Sanoff, of the University of North Carolina, who was not involved in the research, said the study was “small but compelling”.
“These results are cause for great optimism,” she wrote in an editorial accompanying the paper, adding that the research had “provided what may be an early glimpse of a revolutionary treatment shift”.
However, she cautioned that “such an approach cannot yet supplant our current curative treatment approach”, adding that it remains unclear whether the patients are cured.
“Very little is known about the duration of time needed to find out whether a clinical complete response to dostarlimab equates to cure,” Dr Sanoff wrote.
Dr Kimmie Ng, a colorectal cancer expert at Harvard Medical School, told The New York Times the results were “remarkable” and “unprecedented”, but said they would need to be replicated in order to establish their significance.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments