Breakthrough breast cancer blood test proves 100% accurate
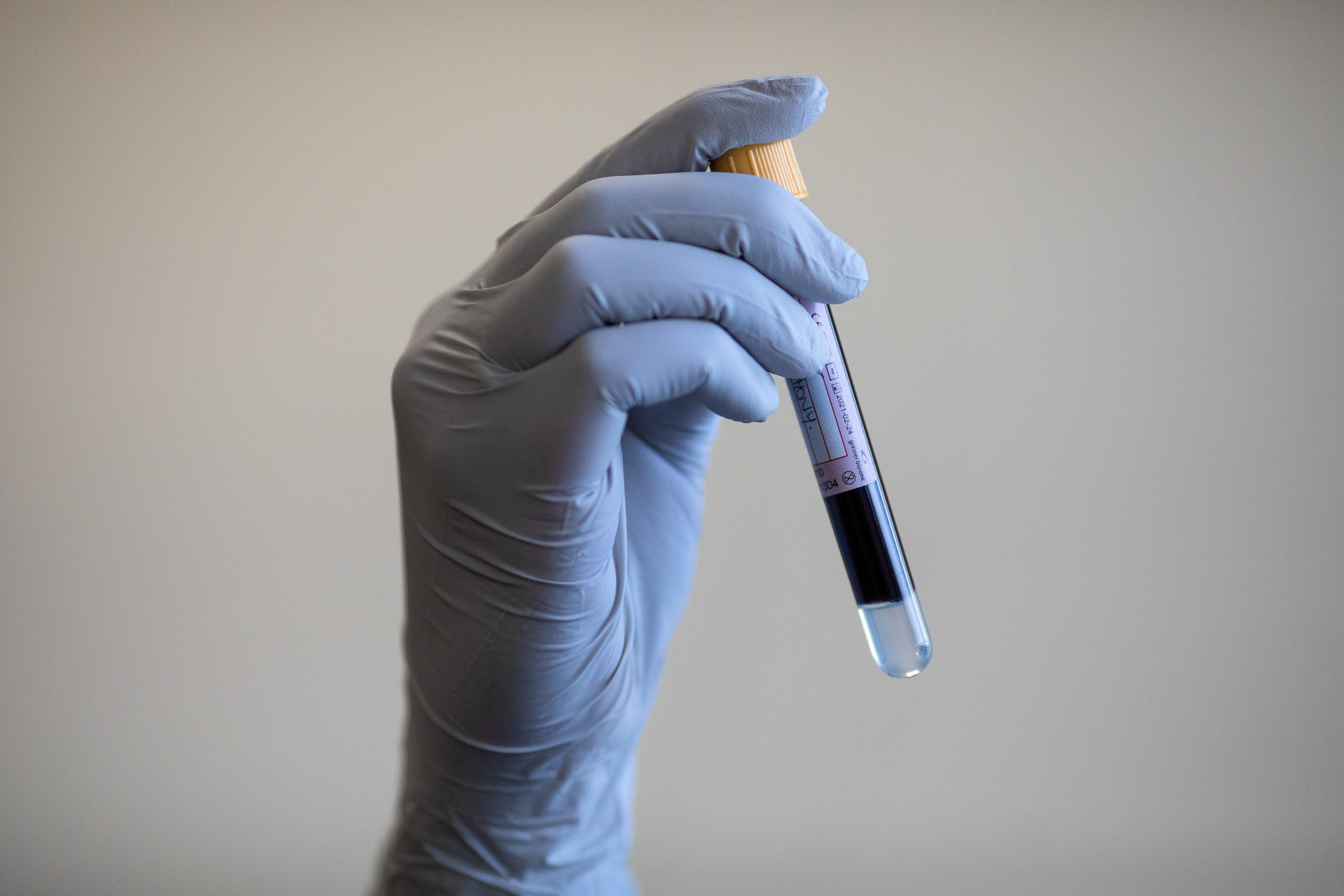
The ‘liquid biopsy’ uses whole genome sequencing to look for genetic faults in a patient’s DNA
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A new blood test can predict if breast cancer will come back years before it shows up on scans.
The “ultra-sensitive” test can pick up traces of a tumour’s DNA ahead of a full relapse, when it is much harder to treat.
It was found to be 100% accurate at predicting which patients would see their cancer come back, paving the way for treatment to start before it becomes incurable.
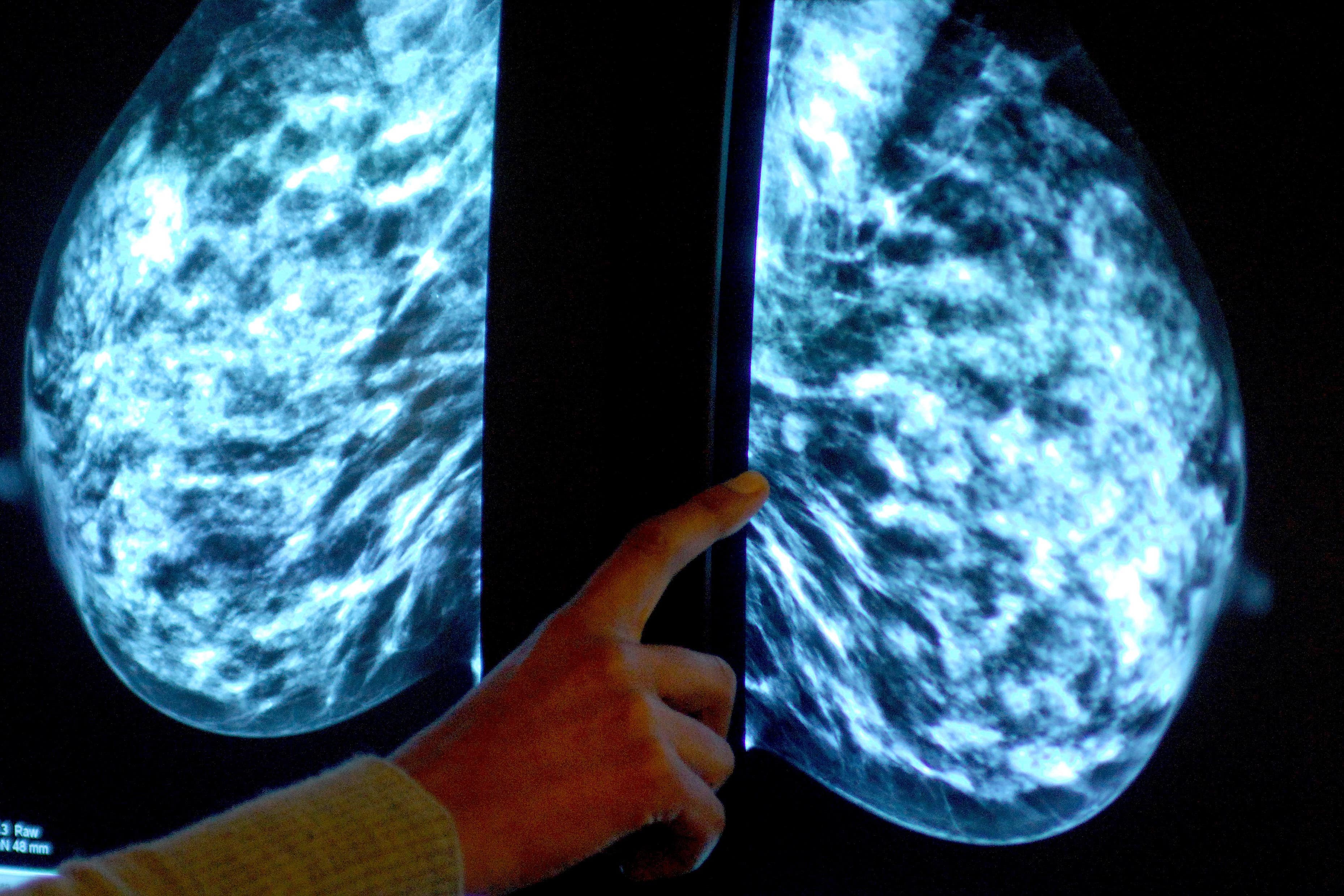
The “liquid biopsy” uses whole genome sequencing to look for genetic faults in a patient’s DNA, which can be a sign of cancer.
A team of researchers from the Institute of Cancer Research (ICR), London, conducted the trial on 78 patients with different types of early breast cancer.
The test looks for 1,800 mutations in the blood which are released by cancer cells, known as circulating tumour DNA (ctDNA).
It successfully found this ctDNA in 11 woman who all went on to see their cancer return. None of the other women relapsed.
Blood samples were tested at the point of diagnosis, then again following surgery and chemotherapy.
These tests were then repeated every three months for the next year and every six months for the next five years.
On average, the blood test detected cancer 15 months before symptoms appeared or it showed up on scans. The earliest was 41 months before a scan confirmed the diagnosis, according to the results presented at the American Society of Clinical Oncology conference in Chicago.
Detection of the tumour DNA at any point after surgery or during the follow-up period saw patients have a higher risk of future relapse and poorer overall survival.
Lead researcher Dr Isaac Garcia-Murillas, from the ICR, said: “Breast cancer cells can remain in the body after surgery and other treatments but there can be so few of these cells that they are undetectable on follow-up scans.”
He added: “These cells can cause breast cancer patients to relapse many years after their initial treatment. Ultra-sensitive blood tests could offer a better approach for the long-term monitoring of patients whose cancer is at high risk of returning.
“Most personalised liquid biopsies currently use whole exome sequencing to identify mutations. But this approach goes one step further and uses whole genome sequencing to identify up to 1,800 mutations in a patient’s tumour DNA that could uniquely identify recurrence of the patient’s cancer from a blood sample.
“A more sensitive test is very important for this group of early breast cancer patients as they tend to have a very low amount of cancer DNA in their blood.
“This proof-of-principle retrospective study lays the groundwork for better post-treatment monitoring and potentially life-extending treatment in patients.”