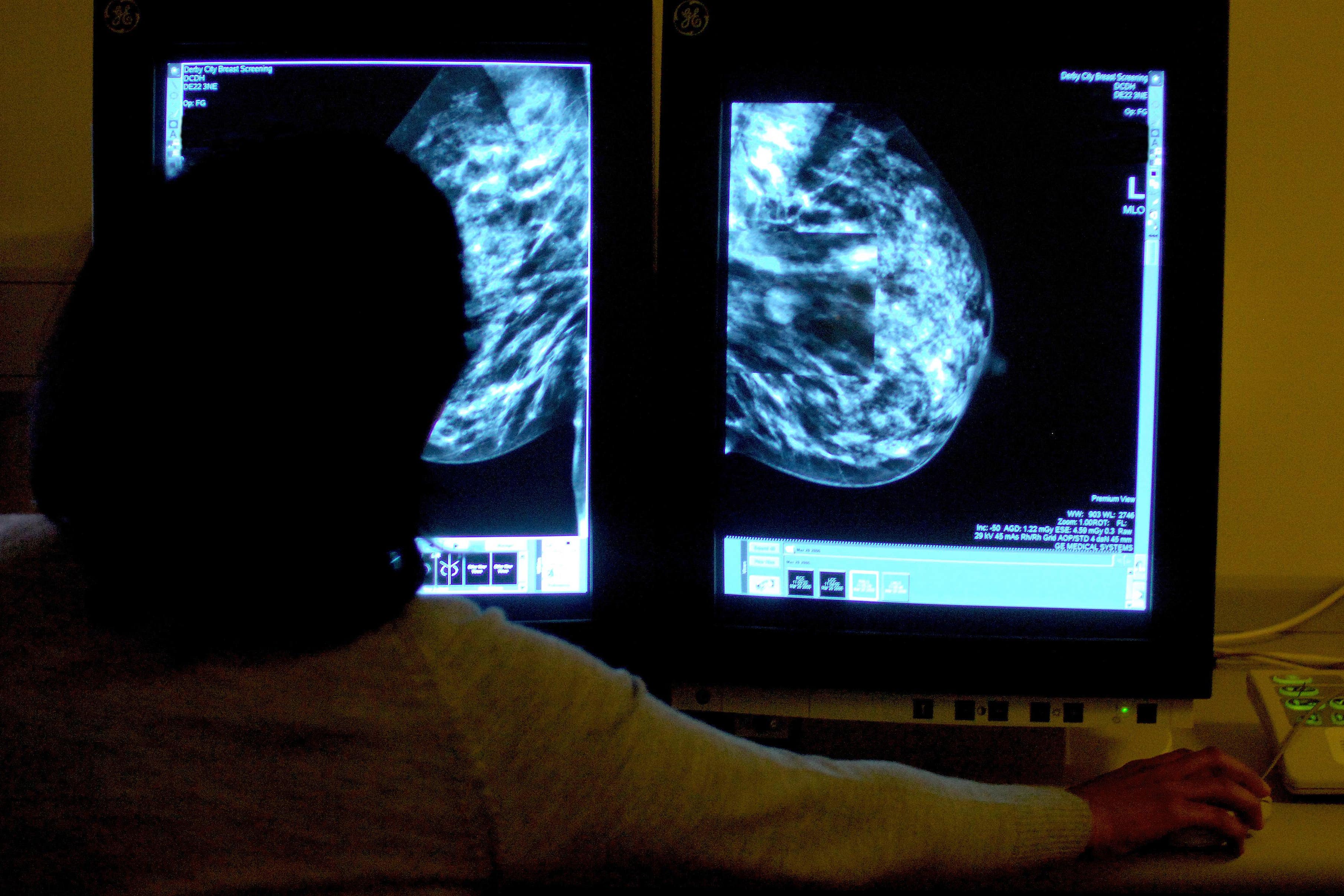
Drugs breakthrough could help those with faulty gene avoid breast cancer surgery
It comes after researchers spotted signs of ‘exhaustion’ in the immune cells of women with the BRCA mutation.
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Giving drugs usually administered in the late stages of breast cancer to healthy people with faulty genes could prevent them from developing the disease, a study has suggested.
The discovery could lead to people who are carriers of the BRCA mutation – which puts them at a higher risk of breast, ovarian and other cancers – being offered preventative treatment options other than surgery, researchers said.
It comes after academics from the University of Cambridge discovered immune cells in the breast tissue of healthy women carrying faulty BRCA1 or BRCA2 genes showed signs of a malfunction known as exhaustion.
This mechanism – usually found in late-stage tumours – suggests the immune cells cannot clear out damaged cells, which eventually leads to cancer.
Drugs already exist that can overcome this block in immune cell function but so far they’ve only been approved for late-stage disease
Senior author Professor Walid Khaled, of the University of Cambridge department of pharmacology and Wellcome-MRC Cambridge Stem Cell Institute, said immunotherapy drugs exist which block this function in the late-stages of the disease.
He said: “We’re very excited about this discovery, because it opens up potential for a preventative treatment other than surgery for carriers of BRCA breast cancer gene mutations.
“Drugs already exist that can overcome this block in immune cell function but so far they’ve only been approved for late-stage disease.”
Immunotherapy helps the immune system recognise and fight cancer. It can be administered on its own or alongside other treatments.
“No-one has really considered using them in a preventative way before,” Prof Khaled added.
“However, these drugs do have serious side effects and we are working now on testing these in pre-clinical models to determine a safe dosage before moving to human studies.”
According to the NHS, out of 100 women with a BRCA1 gene mutation between 65 and 85 will develop breast cancer in their lifetime while between 40 and 63 will develop ovarian cancer.
Out of 100 women with the BRCA2 mutation, between 40 and 85 will develop breast cancer at some point in their life.
In some cases, patients with the faulty genes may be offered risk-reducing surgery, which removes tissue such as breasts or ovaries, that could become cancerous.
Cancer Research UK has granted the Cambridge research team with a Biology to Prevention Award to test the method in mice, and will closely monitor side effects and dosage.
The best weapon we could have against breast cancer is the ability to stop it occurring in the first place
After this, a pilot clinical trial could be carried out in women with BRCA gene mutations.
Prof Khaled added: “The best way to prevent breast cancer is to really understand how it develops in the first place. Then we can identify these early changes and intervene.
“Late-stage breast cancer tends to be very unpredictable and hard to manage. As we make better and better drugs, the tumours just seem to find a way around it.”
Dr Simon Vincent, director of research, support and influencing at Breast Cancer Now, said: “The best weapon we could have against breast cancer is the ability to stop it occurring in the first place.
“This research, which used tissue samples from Breast Cancer Now’s Tissue Bank, suggests that we could prevent some women with altered genes from developing the disease by using drugs currently approved for treatment in the late stages of breast cancer.
“While further research is needed and clinical trials in humans are yet to take place, these findings could be a significant step forward in our care and treatment of people whose genes mean they have an increased risk of developing breast cancer.”
The discovery – published in Nature Genetics – was made as the Cambridge research team was creating an expansive catalogue of human breast cells.
More than 800,000 cells from 55 women are included in the so-called Human Breast Cell Atlas, which will be made available for other researchers to use and add to.
It also contains information on other risk factors for breast cancer, such as body mass index (BMI), contraceptive use, alcohol consumption and menopausal status.
Austin Reed, a PhD student in the University of Cambridge’s department of pharmacology, said: “We’ve found that there are multiple breast cell types that change with pregnancy, and with age, and it’s the combination of these effects – and others – that drives the overall risk of breast cancer.
“As we collect more of this type of information from samples around the world, we can learn more about how breast cancer develops and the impact of different risk factors – with the aim of improving treatment.”