Red light can reduce blood glucose levels, new study suggests
The study was conducted in healthy people, but the technique could potentially impact diabetes control after meals, researchers say.
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Shining a red light on a person’s back can help reduce blood sugar levels, new research suggests.
According to the findings, a specific frequency of the light used for 15 minutes led to a 27.7% reduction in blood sugar levels after taking glucose (sugar), and it reduced maximum glucose spiking by 7.5%.
Spikes are a rapid increase in the amount of sugar in the blood, after eating specific foods.
The experts suggest their findings also indicate significant long-term consequences for human health, including the potential for blood sugar to be negatively influenced by lengthy exposure to blue light.
Our study has shown that we can use a single, 15-minute exposure to red light to reduce blood sugar levels after eating
Given the prominence of LED lighting in modern life, and the fact that they emit towards the blue end of the light spectrum with very little red, the authors say this may be a potential “health span time bomb”.
The scientists suggest blue light on its own can drive disrupted blood sugars that may in the long run contribute to diabetes and undermine health spans.
But this can be partly addressed through spending more time in sunlight, they add.
Although the study was conducted in healthy people, the technique could potentially impact diabetes control after meals, as it can reduce damaging fluctuations of blood glucose that contribute to ageing.
Lead author of the study, Dr Michael Powner, senior lecturer in neurobiology at City, University of London, said: “It is clear that light affects the way mitochondria function and this impacts our bodies at a cellular and physiological level.
“Our study has shown that we can use a single, 15-minute exposure to red light to reduce blood sugar levels after eating.
“While this has only been done in healthy individuals in this paper, it has the potential to impact diabetes control going forward, as it could help to reduce potentially damaging glucose spikes in the body after meals.”
Professor Glen Jeffery, Professor of Neuroscience in the UCL Institute of Ophthalmology, said: “Sunlight has a balance between red and blue, but we now live in a world where blue light is dominant because although we do not see it, LED lights are dominant in blue and have almost no red in them.
Long-term exposure to blue light is potentially toxic without red. Blue light on its own impacts badly on physiology and can drive disrupted blood sugars that may in the long run contribute to diabetes and undermine health spans
“This reduces mitochondrial function and ATP production. Hence our internal environments are red-starved.
“Long-term exposure to blue light is potentially toxic without red. Blue light on its own impacts badly on physiology and can drive disrupted blood sugars that may in the long run contribute to diabetes and undermine health spans.
“Pre-1990, we all had incandescent lighting which was okay because it had the balance of blue and red similar to sunlight, but there is a potential health span time bomb in the change to LEDs in an ageing population.
“This can partly be corrected by spending more time in sunlight.”
The study found that at a frequency of 670 nanometers (nm) red light stimulated energy production within mitochondria, the tiny powerhouses within cells, leading to increased consumption of glucose.
In previous studies, 670 nm light shone selectively onto the backs of mice showed improvement of a molecule, called adenosine triphosphate (ATP), that improves symptoms in both a model of Parkinson’s disease, and a model of diabetic retinopathy – loss of vision in people with diabetes.
Previous research established that long wavelength light between approximately 650-900 nm can increase production of ATP which reduces blood glucose and also improves health/lifespan in animals.
In the study, researchers recruited 30 healthy people, who were put into two groups – 15 in the 670 nm red light group, and 15 in the no light group.
If confirmed later in people with diabetes, this could be the foundation of a useful intervention
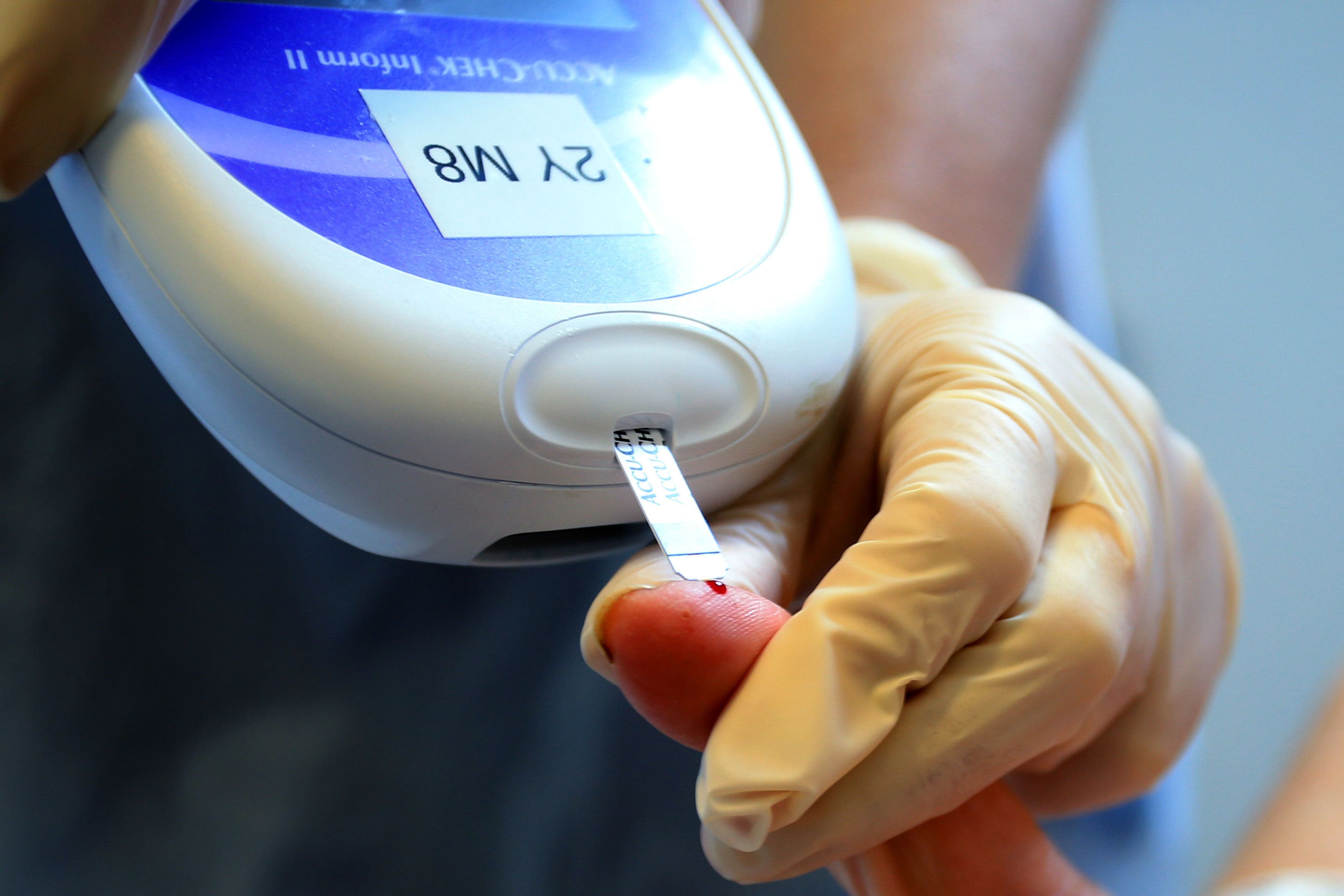
They were then asked to drink glucose dissolved in water and record their blood glucose levels every 15 minutes over the next two hours.
People who received red light exposure 45 minutes before having the drink exhibited a reduced peak blood glucose level and reduced total blood glucose during the two hours.
The study, published in the Journal of Biophotonics, was sponsored by Sight Research UK.
Keith Frayn, emeritus professor of human metabolism, and emeritus fellow at Green Templeton College, University of Oxford, said: “If confirmed later in people with diabetes, this could be the foundation of a useful intervention.
“But these intriguing findings should be regarded as quite preliminary.
“More investigations would be needed before we can fully assess this effect.
“Importantly, we need to know whether this is a true metabolic effect, or whether, for instance, the warming effect of the red light exposure alters patterns of blood flow, potentially altering the nature of the blood sampled by pricking a finger.
“We also need more information on what happens to the glucose that doesn’t appear in the blood.”