Ambulance response times double as patients die waiting for paramedics
Ambulance trusts see spike in deaths as flood of 999 calls and hospital delays hit response times
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Patients are waiting almost twice as long for a paramedic as they were at the height of the pandemic, The Independent can reveal, as ambulance services buckle under the strain of record demand with dwindling resources.
Response times for all types of emergency – including life-threatening – are at their highest on record with patients dying before paramedics can reach them.
An investigation by The Independent has found a 26 per cent spike in the most serious incidents reported by paramedics so far in 2021 compared to the whole 12 months of 2019, before the Covid-19 pandemic began.
With several months of 2021 left to run, deaths as a result of safety incidents in ambulance trusts are up 13 per cent compared to 2019.
All 10 of England’s NHS ambulance trusts have raised their alert levels to their highest point, with some having been on what was previously called “black alert” since the beginning of the summer. Many have repeatedly declared critical incidents and ministers called in the military earlier in the summer, with soldiers driving ambulances to try and meet the record numbers of 999 calls.
A number of frontline paramedics have spoken out over the “heart-wrenching” sense of failure they feel at finding patients have died before they could reach them.
‘Unimaginable distress’
Now the head of the care watchdog has told The Independent he has “very real concerns” for the safety of patients, warning some are being left in pain for hours or deteriorating before help arrives.
Professor Ted Baker, chief inspector for the Care Quality Commission, said it was clear increasing numbers of patients were needing emergency care, describing pressure on the NHS as severe.
He said patients were facing “unacceptably long delays” for ambulances and admission to hospital.
“There are very real concerns about the risk to patients – with reports of people left in significant pain for hours or whose health deteriorated before paramedics were able to attend”, he said, adding: “The impact of these mounting pressures on staff in ambulance services and hospitals is also a major concern as they do all they can to deliver safe care under the most demanding circumstances.”
Prof Baker said the problems with capacity in the NHS had been building for years but had been made worse by the pandemic. “There are no simple solutions”, he said, adding that new models of care would ultimately be needed in the future.
Serious incident reports filed by ambulance service staff show Prof Baker’s concerns for safety are valid.
There were 263 severe harm incidents – which involve permanent harm – or deaths reported to NHS England by ambulance trusts for the period January to December 2019.
For January to August 2021, there were 333 severe harm and death incidents reported – a 26 per cent rise on 2019, with four months of data still to be reported.
For deaths alone, the numbers are up 13 per cent in January to August 2021, compared to the full year of 2019, again with four months of data still to be reported.
Across the whole pandemic, since April 2020 there have been 533 severe harm and death incidents up to August 2021.
Not all of the incidents will relate to ambulance delays but the majority of reported incidents are categorised as incidents relating to access, admission and transfers of patients.
Shadow health secretary Jonathan Ashworth told The Independent: “Over a decade of failure to invest in the ambulance workforce, including recruiting paramedics, call handlers, and support staff is now leaving patients in pain and unimaginable distress, unable to get the help they need.
"NHS staff are already stretched to breaking point, burnt out and exhausted. Ministers need to support them with a proper plan to ensure our ambulances can continue their vital work this winter.”
‘The sense of failure is huge’
The pressure on ambulance service staff working on the front line has been relentless for months now, as ambulance services dealt with their busiest ever summer, with a record one million 999 calls in July alone.
One paramedic from the South East Coast Ambulance Service told The Independent they responded to a 999 call for a patient struggling to breathe. They arrived 52 minutes later but the patient had already died.
“If we had met the target time, that could have been avoided. The patient was on their own. When we got there, things had been spilt and knocked over, it was clear they had been in some distress. We had a sense of their panic and of being alone and dying alone.
“The sense of failure is huge. It’s heart-wrenching.”
They added: “Another patient in their nineties fell while out walking at night and was found by a member of the public after a fall at midnight. He waited over seven hours in the cold for an ambulance, with rib fractures.
“We get to these patients and they are suffering, not from their injuries but from the waits. Another lady who fell at home waited over six hours for an ambulance and had to be taken to hospital, not because of the fall but because of the effect of being left on the floor for so long.”
The paramedic said they believe the entire ambulance service was in the grip of a major incident but added the NHS management were “tolerating poor care. It’s just become accepted.”
This story is being repeated across England with reports of patients dying in the backs of ambulances and elderly patients lying on the floor for hours after calling 999.
Analysis of the latest NHS England ambulance data by law firm Bond Turner shows the significant decline in performance. The firm found 999 calls for an ambulance were up 33 per cent in the 12 months to September, with the average wait time for an ambulance at 1 hour and 17 minutes, an increase of 88 per cent on 2020 and more than double the wait in 2019.
Response times for life-threatening calls have increased 26 per cent to nine minutes, one minute longer than the eight-minute target.
NHS data shows response times for every severity of call are the longest since data was first collected across England in 2018.
Patients in the southwest of England are facing the longest response delays on average, at 1 hour and 35 minutes, while the Midlands saw the highest year-on-year increase in ambulance waiting times, up 160 per cent from 49 minutes to 1 hour 20 minutes.
For the longest waits, patients in London have seen waiting time soar from 55 minutes to over four hours.
Sara Stanger, head of clinical negligence at Bond Turner, said: “Having to dial 999 and request an ambulance for a family member, a friend or ourselves is already an extremely stressful situation, but a long wait adds a huge amount of pressure and anxiety.
“Of course, these delays lead to potential patient care and health repercussions, which can sometimes be very serious, and this is despite staff working tirelessly to try and alleviate this crisis.”
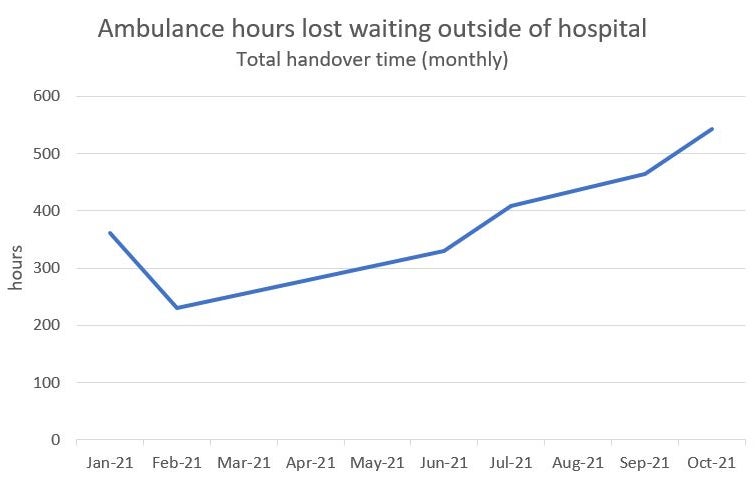
Data obtained by The Independent shows in October ambulances across the West Midlands region were delayed outside hospitals by a total of 28,000 hours – which resulted in 78 ambulance crews not able to respond to 999 calls.
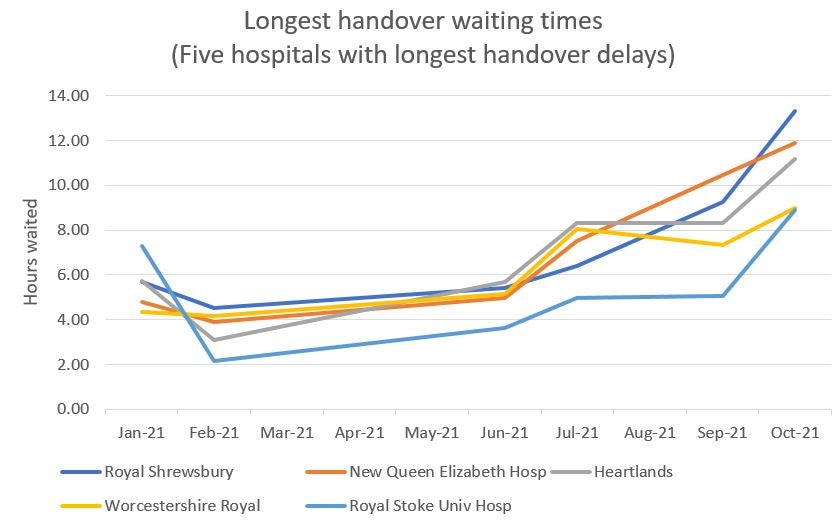
One patient at the Royal Shrewsbury Hospital, in Shropshire, waited 13 hours in the back of an ambulance that month, and records show waits of more than 10 hours across hospitals in Birmingham.
The Independent has also seen data for the Yorkshire Ambulance Service revealing “category two” patients, who should be reached within 18 minutes, have been left waiting nearly 50 minutes on average last month. Some waited an hour and 15 minutes. These patients could be suffering from a stroke or suspected heart attack.
One paramedic working for the Yorkshire Ambulance Service said: “I just really fear for patient safety and for staff welfare; I’ve never seen anything like this for such a sustained period. Demand is far exceeding supply a lot of the time for a number of reasons; it’s complex.”
In London, the Ambulance Service has been at level four or “black alert’ since mid-June due to significant demand. It has been receiving around 2,000 more calls each day compared to before the pandemic, when they received 5,000 a day on average.
According to leaked data for this past week, category two patients in the capital were waiting a similar length to those in Yorkshire. Data showed the services response times for category two patients had deteriorated from 20 minutes in June to 50 in October.
On Tuesday afternoon, the service had to place 262 emergency calls on hold as there was no ambulance to send. A large proportion of these were seriously ill (category 2) patients.
Richard Webber, from the College of Paramedics, told The Independent: “Paramedics from across the country are saying they’re going to more and more patients who’ve waited far too long for help and those patients have either deteriorated or died as a result of delays.”
He said: “There’s been a couple of cases recently where patients have been in an ambulance outside of hospital and then stopped breathing and have subsequently died. In the past those patients would’ve been in hospital. Would they have died or not it’s really hard to tell, but they would’ve been in an emergency department being treated.”
He added: “It’s not the A&Es’ fault, it’s the whole system’s fault” and emphasised the situation was very “distressing” for ambulance staff, who are now facing increased incidents of abuse from the public due to long waits.
‘Some patients die in front of us’
This week, a coroner for Stoke-on-Trent ruled one man had died as a result of a “gross failure of care” in July, after paramedics took nine hours to respond to a 999 call.
Paramedics found Shaun Mansell, a 50-year-old, dead in his home on 5 July after his neighbour called for an ambulance as he was suffering from shortness of breath.
Speaking anonymously with The Independent, one paramedic from the east of England said: “The hospitals grind to a halt because there’s no space and no beds. A&E staff work so hard but they’re short staffed so it’s inefficient, there’s sometimes one nurse managing the handover area and there’s only so much they can do.
“We end up doing ‘corridor nursing’ to monitor patients. Even time-critical patients with potential to deteriorate have to wait. Some have been known to die in front of us, but it doesn’t get spoken of due to patient confidentiality.”
Pressures in the ambulance service are also having a knock-on impact in other parts of the NHS, with GPs having to provide care for waiting patients.
Dr Becky Haines, a senior GP in Gateshead, said on Twitter this week: “At one point last week, my colleagues at the practice had three patients on oxygen waiting for urgent ambulances. We are not a large practice, and our nurses were worried we would run out of oxygen. We’re now discussing increasing our oxygen supplies.”
Another GP in London said they had the same issue two weeks ago, almost using up two tanks of oxygen waiting for a category two ambulance to arrive.
North West Ambulance Service said it had been at extreme pressure, or level four, since 7 September and was receiving 5,000 emergency calls a day. Of these the most serious life-threatening category 1 and 2 calls made up 72 per cent of all calls in October.
South Central Ambulance Service declared a critical incident recently over the demand it has seen from patients with 999 calls 13 per cent above 2019, the equivalent of 6,500 more call-outs.
In the southwest region, a spokesperson for the ambulance service said it was experiencing its “highest ever level” of demand, with a new 999 call coming every 27 seconds while delays at hospital were longer than it had ever seen before.
The service has been at level four extreme pressure since 14 June.
The spokesperson added: “We are losing many more hours compared with recent years which causes our ambulances to queue outside hospitals and unable to respond to other patients and has an inevitable impact on the service we can provide. This is a system problem which therefore demands a system solution.”
An NHS England spokesperson said: “Staff have gone above and beyond over the last year contending with record levels of A&E attendances and ambulance call outs, all while treating more than 470,000 seriously ill covid patients, and this has inevitably lead to increased pressure on ambulance services.
“This is why the NHS set out a 10-point action plan to prepare for significant demand this winter and also wrote to trusts and systems asking for handover delays to be avoided with immediate effect in order to get crews responding quicker.”

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments