Breakthrough Alzheimer’s blood test could detect disease 15 years before symptoms emerge
Simple procedure could lead to a national screening programme for everyone aged over 50, say experts
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A simple blood test can detect Alzheimer’s up to 15 years before symptoms emerge, with experts claiming it could “revolutionise” early diagnosis of the disease.
Swedish trials found the test to be as accurate at detecting the signs of Alzheimer’s as painful lumbar punctures, and better than a range of other tests currently being worked on.
Experts say it could pave the way for a national screening programme for the over-50s, and that current treatments could work better with the cases picked up earlier.
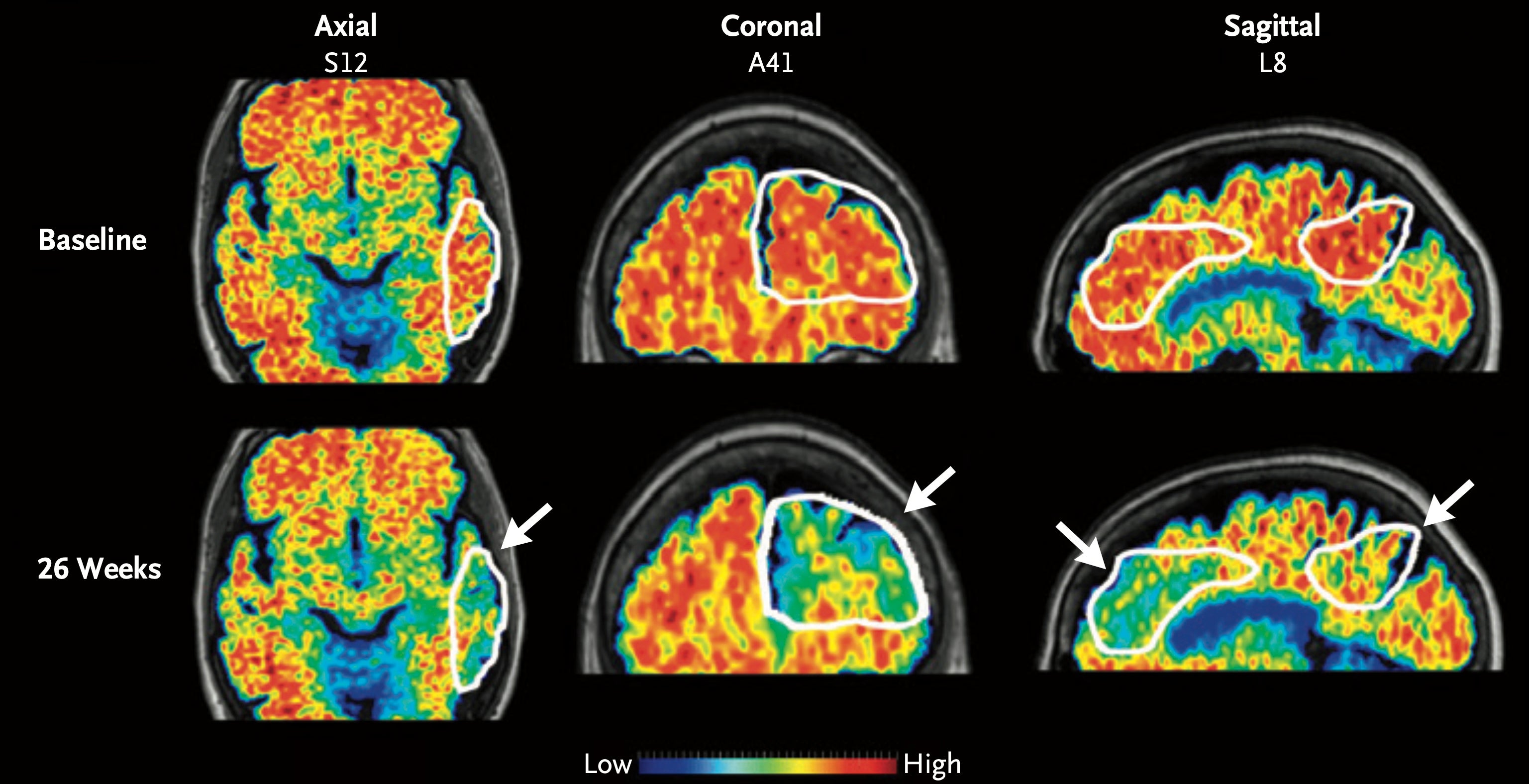
The test works by measuring levels of a protein called p-tau217 in the blood that indicate biological changes taking place in the brain during Alzheimer’s disease.
It could identify patients as likely, intermediate or unlikely to have Alzheimer’s disease and potentially rule out the need for further, more invasive investigations.
Prof David Curtis, honorary professor, UCL Genetics Institute, University College London, said: “Everybody over 50 could be routinely screened every few years, in much the same way as they are now screened for high cholesterol.
“It is possible that currently available treatments for Alzheimer’s disease would work better in those diagnosed early in this way. However, I think the real hope is that better treatments can also be developed.
“The combination of a simple screening test with an effective treatment for Alzheimer’s disease would have a dramatic impact for individuals and for society.”
The test is made by company ALZpath and is already commercially available.
In the trial of 786 people – conducted by Dr Nicholas Ashton at the University of Gothenburg, and colleagues, and published in the Jama Neurology journal – the researchers were able to use it to categorise a patient’s likelihood of having Alzheimer’s.
The higher the levels of p-tau217 in the blood, the more likely or advanced the disease was.
A University College London-led study has claimed the test could detect the first signs of the disease up to 15 years before symptoms start showing.
Dr Sheona Scales, director of research at Alzheimer’s Research UK, said the study “adds to a growing body of evidence that this particular test has huge potential to revolutionise diagnosis for people with suspected Alzheimer’s”.
Currently, the only way to prove that someone has a build-up of the proteins in the brain is to have a lumbar puncture, which involves a needle being inserted into the lower back, or a scan available in only about one in 20 NHS memory clinics.
Dr Richard Oakley, associate director of research and innovation at the Alzheimer’s Society, said: “This study is a hugely welcome step in the right direction as it shows that blood tests can be just as accurate as more invasive and expensive tests at predicting if someone has features of Alzheimer’s disease in their brain.
“Furthermore, it suggests results from these tests could be clear enough to not require further follow-up investigations for some people living with Alzheimer’s disease, which could speed up the diagnosis pathway significantly in future.
“However, we still need to see more research across different communities to understand how effective these blood tests are across everyone who lives with Alzheimer’s disease.”
One in three people born in the UK today will develop dementia in their lifetime, according to the Alzheimer’s Society, which estimates around 900,000 people are living with the disease. The charity believes this will rise to 1.6 million people by 2040.

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments