More than 160 million women across the world have unmet contraception needs, study finds
Women in south Sudan – where just two per cent have access – are most affected

More than 160 million women across the world have unmet contraception needs, new research has found.
Younger women and those living in sub-Sarah Africa and south Asia were the most affected, according to the largest study of its kind, which was published in The Lancet journal.
Researchers analysed data from 1,192 surveys to produce national estimates on the proportion of women of reproductive age (15-49) using contraceptive methods, the types of contraceptives being used, and unmet needs for contraception.
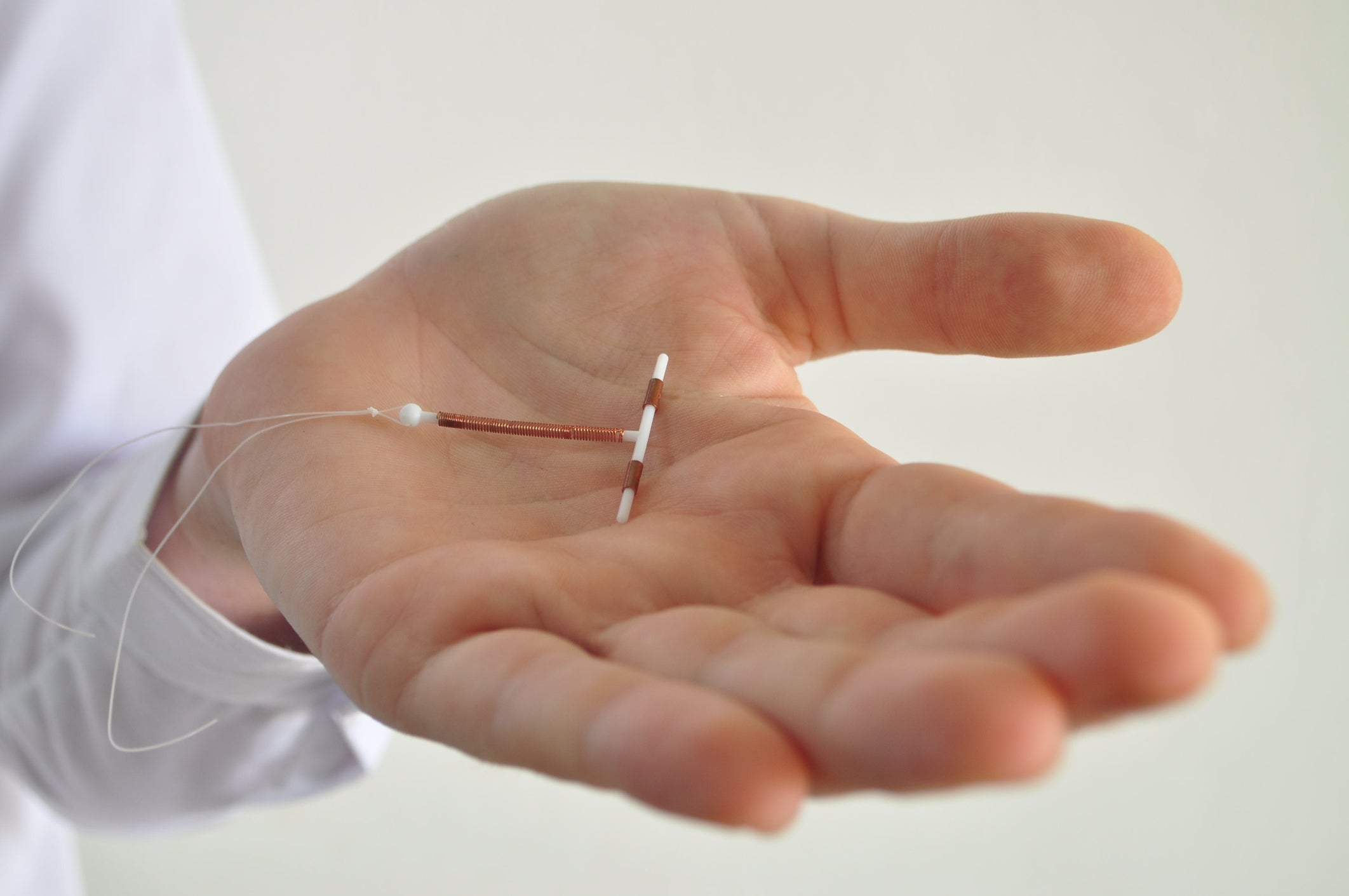
The use of contraception has significantly increased since 1970, driven by the availability of “modern” contraceptive methods such as oral contraceptive pills, IUDs, as well as male and female sterilisation.
While the share of women using modern contraception has risen from 28 per cent in 1970 to 48 per cent in 2019, there remain gaps in accessibility.
As of 2019, 163 million women who needed contraception were unable to access it.
Dr Annie Haakenstad, a professor the Institute for Health Metrics and Evaluation at the University of Washington and an author of the study, commented: “Although we’ve observed excellent strides in contraceptive availability since the 1970s at a global level, there’s still a long way to go to ensure that every woman and adolescent girl can benefit from the economic and social empowerment contraceptives can offer.
“Our results indicate that where a woman lives in the world and their age still significantly impacts their use of contraception.”
The study highlights significant differences between use of contraception across different countries.
Southeast Asia, east Asia and Oceanis had the highest use of modern contraceptives (65 per cent), with 90 per cent of women reporting that their need for contraception was satisfied.
Sub-Saharan Africa had the lowest use of modern contraceptives (24 per cent) and only 52 per cent of demand was satisfied.
The statistics were the lowest in southern Sudan, where contraception was used by just two per cent of women, and highest in Norway, where it was used by 88 per cent.
There were also disparities by age group. Women and adolescents in the 15-19 and 20-24 age groups have the lowest rates of demand satisfied globally – estimated at 65 per cent and 72 per cent, respectively.
Those aged between 15 and 24 represent 16 per cent of total need, but 27 per cent of this group’s needs are not being met. This amounted to 43 million young women not having access to contraceptives they needed in 2019.
“Our study calls attention to young women being overrepresented among those who cannot access contraception when they need it,” Haakenstad said.
“These are the women who stand most to gain from contraceptive use, as delaying having children can help women stay in school or get other training opportunities and to enter and maintain paid employment.
“This can lead to social and economic benefits that last throughout a woman’s lifetime and is an essential driver towards greater gender equity.”
One key factor behind the unmet demand is a lack of variety in contraceptive methods.
In Asia, female sterilisation made up more than half of all contraceptives used in south Asia. In high income countries, the oral contraceptive pill and condoms were most dominant.
“Our study highlights that not only should contraception be available to all women, but also suitable choices of contraceptives,” Professor Rafael Lozano of the University of Washington, an author of the study, said.
“Diversifying options in areas that may be over-reliant on one method could help increase contraceptive use, particularly when the most used method is permanent.
“To widen access, we urge policymakers to use these estimates to look at how contraceptive choice interacts with age and marital status in their countries.”



Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments