The Independent's journalism is supported by our readers. When you purchase through links on our site, we may earn commission.
What happens to your body when it doesn’t get enough calcium?
Rickets was a common problem in the Victorian days, but the condition could be on the rise again

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.If you grew up in an era where you were encouraged to enjoy a free bottle of milk at school break-time, the importance of getting plenty of calcium is probably one of the earliest and most prominent healthy eating messages you remember.
From a young age, most of us have had the crucial role it plays in bone strength strongly instilled in us. However, it has lots of other responsibilities too.
You’d probably not be surprised to hear that about 99 per cent of your body’s calcium lives in your bones, with some in your teeth too. The small quantity that remains is put to work in your bodily fluids and soft tissue.
In addition to its role within the skeleton, it is crucial to muscle contraction, which includes the muscles of our hearts, nerve communication and blood clotting.
How much calcium do I need?
The human body needs a huge variety of nutrients, but calcium is certainly the mineral you would find in most abundance. As an adult, you would expect to find 1200 grams of calcium in your bones. This could equate to as much as two percent of your overall body mass.
It can be fairly easy to get enough calcium from your diet to keep your bones and the rest of your body satisfied. The amount you need to consume depends on your age, size and medical factors, but most adults need at least 700 milligrams a day.
Your body may demand more though. Pregnant and breastfeeding women, for example, usually need to increase their intake to meet their own needs and that of their baby. Higher amounts are also required during adolescence.
This super nutrient also has an important ally – vitamin D, which is vital for your body to absorb and retain calcium. It is estimated that one in five adults and one in six children in the UK have low vitamin D levels, with guidance from the National Institute for Health and Care Excellence (NICE) suggesting better access to dietary supplements for those at risk.
There are plenty of natural sources of both calcium and vitamin D though. While most of our vitamin D comes from exposure to sunlight, dairy-based products are often the richest sources of calcium in our diets. However other foods providing calcium include sardines with bones, spring greens and leafy green vegetables, nuts, tofu and oranges.

The dangers of low calcium
A deficiency in early years can make children susceptible to Rickets, where bones become soft and weak. Vitamin D deficiency and calcium are both key factors and can result in permanent bone deformities. Rickets was a common problem in the Victorian days, but there has been suggestion that the condition could be on the rise again.
People who’ve had low calcium levels are at risk of experiencing problems with their bones in later life, making them more susceptible to bone fractures.
Although you stop growing in height during your teenage years, your bone density should actually continue to strengthen through to your late twenties. Bone density generally starts to decrease in your thirties and for women there is usually a rapid deterioration after the menopause. It is beneficial for your bone mass to be at its peak, before this natural decline begins.
Osteoporosis, a condition characterised by fragile bones, is a common problem. In the UK it affects around three million people and is responsible for around 300,000 broken bones each year.
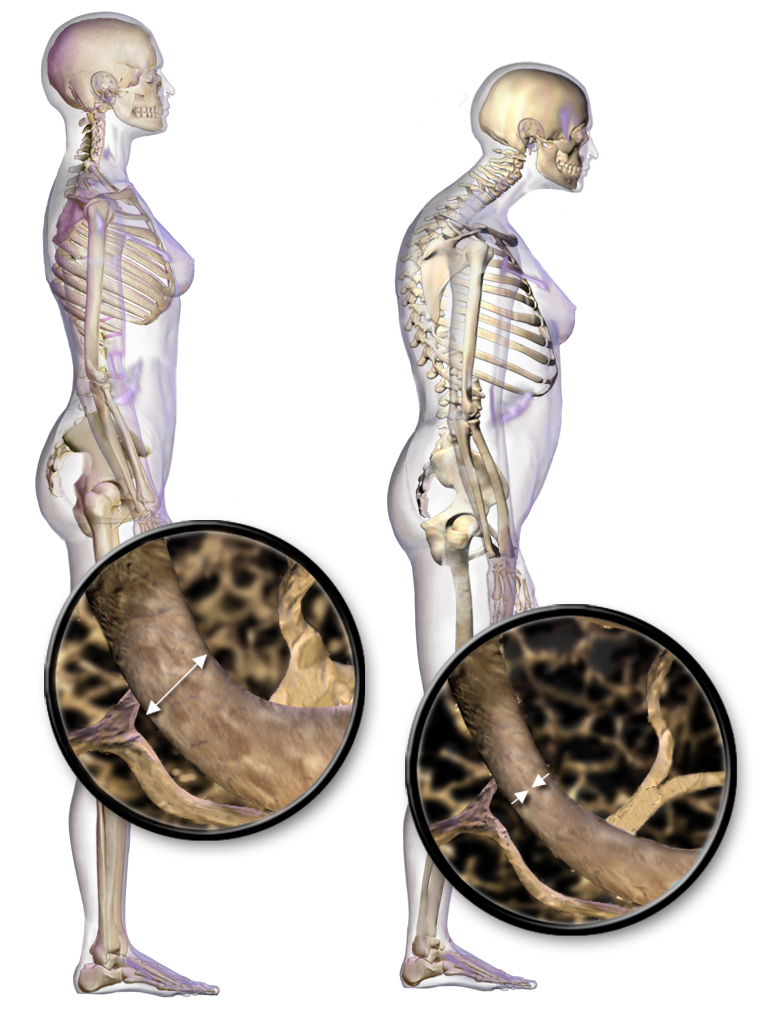
There are no outward symptoms of osteoporosis but there are key risk factors that your doctor will be on the look out for. Some of these factors are unavoidable and cannot be changed, such as a family history and an early menopause. However there are factors such long term use of medications such as steroids, excess alcohol use, smoking, as well as calcium and vitamin D deficiency, that are modifiable. As part of the treatment plan for patients in osteoporosis, doctors will usually recommend regular calcium and vitamin D supplements.
Most of the calcium in our bodies will be used for our bone growth and strength, with a small but important percentage being directed elsewhere for essential functions like regulating blood pressure, contracting muscles and transmitting nerve signals. If your diet isn’t delivering a ready supply for these important processes, the calcium will start to be extracted from your bones having a further negative impact on their strength.
Silent symptoms
Whilst the importance of calcium is clear, the physical signs that you could be deficient are not always so obvious. Symptoms of low calcium levels (hypocalcaemia) often occur late on and can include involuntary muscle twitches called tetany, altered sensation around the mouth and petechiae (a red or purple coloured rash). Calcium levels can be checked with a blood test.
Your doctor may suggest performing X-rays or a more specialised form of imaging by arranging a dual-energy X-ray absorptiometry (DXA) scan. These scans can assess the density of bones and is the gold-standard for diagnosing conditions such as osteoporosis.
Calcium supplements are a common treatment and often suggested for post-menopausal women and the elderly. However, it is generally not recommended to take more than 1500 milligrams a day in supplement form, as this can cause stomach pain and diarrhoea.
There has been speculation over a possible link with calcium tablets and cardiovascular problems. Although a study published in the Heart journal suggested there could be an association, a direct link has not been proven. If you have any concerns about supplements your GP has suggested, you should discuss these with them.
For those wanting to boost their calcium intake through their diet, there are plenty of natural sources to choose from. So even if you were one of the kids in class who hated their daily dose of milk, you should be able to find more tempting choices to boost your calcium levels.
Dr Alexandra Phelan is an NHS GP and member of the Pharmacy2u.co.uk Online Doctor Service team
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments