The possible outcomes for victims of the tainted blood scandal, 40 years on
A public inquiry into the infected blood scandal will identify where fault lies, but what reparations are the courts able to provide?
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Following the announcement of a public inquiry into the blood contamination scandal of the 1980s, a court has now ruled that surviving victims may sue the Government to obtain compensation. After decades, the thousands of victims and their families will feel they have finally been given an opportunity to obtain justice.
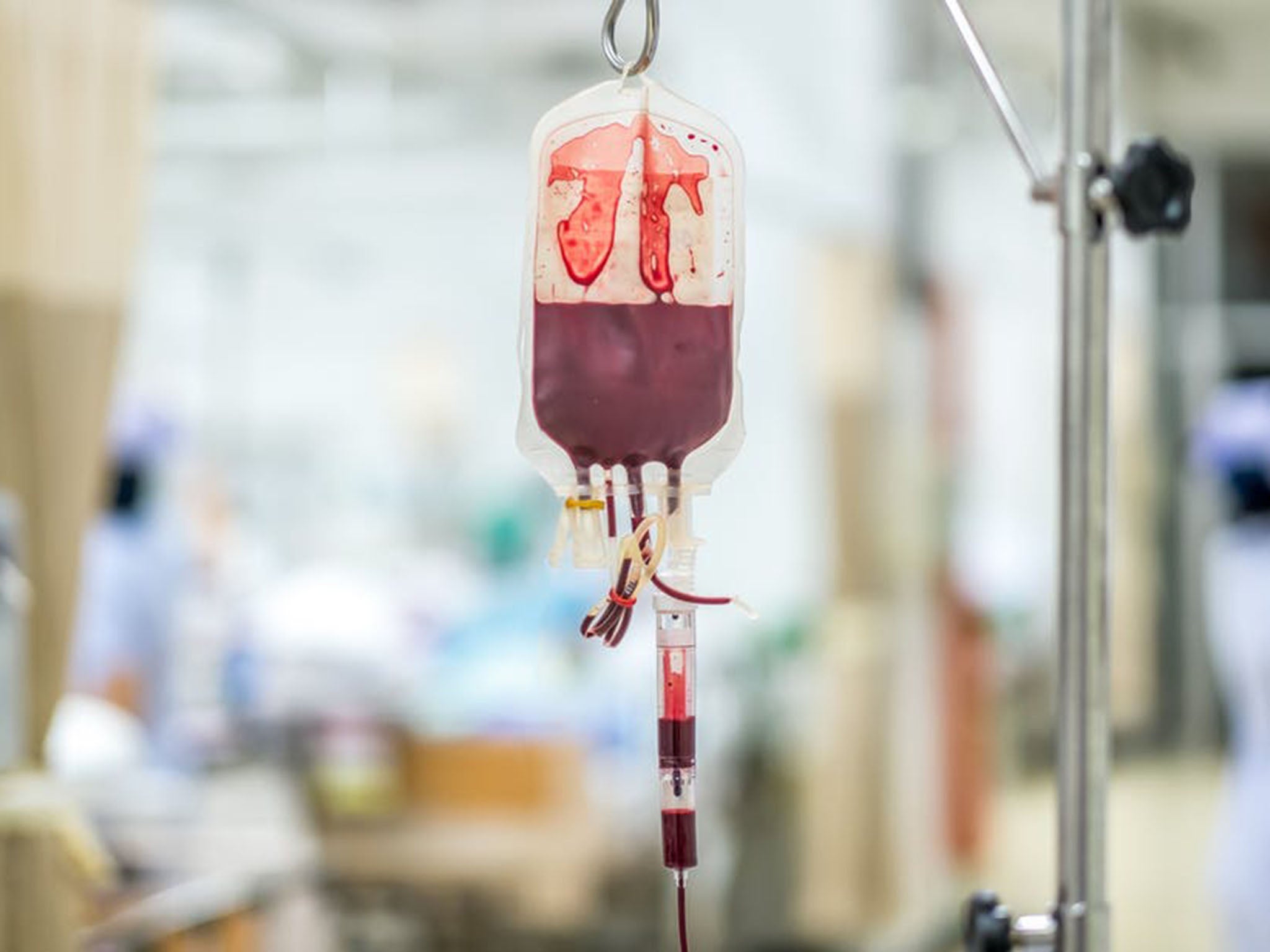
About 5,000 people with haemophilia became infected with hepatitis C and HIV following treatment with contaminated blood products between the 1970s and early 1990s as a result of negligence and failings by health authorities. At least 2,400 have since died, but until now there has been no public inquiry into the scandal, or no real opportunity to obtain financial compensation for the harm caused.
The issue began with the development of concentrated blood clotting factors in the 1970s – products derived from blood that proved transformative to patients with haemophilia, allowing them to lead relatively normal lives. Health authorities all over the world aimed for self-sufficiency in blood-based products, but the UK was slow to do so. Instead, it relied on imports from the US, many of which were manufactured from blood plasma drawn from thousands of paid donors. These included products coming from high-risk populations, such as prisoners and drug addicts, where hepatitis C and HIV were more common. While Scotland became largely self-sufficient, the rest of Britain still imported most of its supply from the US during the 1980s – when the risk of HIV was at its greatest.
The dangers of blood contamination were well understood at the time – and donor screening, HIV testing and heat treatment were recommended by scientists worldwide. But these precautions were not taken up quickly enough in the UK – often because of costs – meaning patients were exposed to unnecessary risks.
Victims and their families have fought for decades to get to the bottom of how such a failure could have happened, yet to date no individual or public authority has been held accountable. Victims were instead offered minimal “ex-gratia payments” on condition that they dropped their claims.
Other countries took a different approach: in France, for example, more than 30 people including blood centre officials, doctors and ministers were prosecuted for criminal offences including negligence and deception – and two senior officials were jailed.
So the announcement of an inquiry by Prime Minister Theresa May, after years of pressure from MPs and campaign groups, including Greater Manchester mayor Andy Burnham – who has even claimed there is evidence of a “criminal cover-up” – has been seen as a last chance for those affected.
The battle for a public inquiry
The inquiry’s aim is to investigate the failings of authorities at the time. Criminal proceedings may follow if there is evidence of criminal conduct. It has been a long time coming. Lobbying by victims of the contamination for compensation started in England in 1987, with demands for a public inquiry the following year. Resistance in Westminster to launch a public inquiry was reflected in the following statement by Lord Warner, then minister of state for health, in 2006: “We do not consider that a public inquiry is justified as we do not believe that any new light will be shed on this issue as a result.”
Yet the Archer Inquiry, an independent report funded by donations, and so not a formal public inquiry, published a report in 2009 that stated “there was something to hide” and that “secrecy fosters suspicion”. Following devolution the Scottish Executive held the Penrose Inquiry into the scandal, which reported in 2015 and made a number of recommendations to ensure blood safety in Scotland, but was angrily dismissed by campaigners as “a waste of time and money” for failing to apportion blame. Successive governments in Westminster have failed to act on what was a national scandal.
What are the possible outcomes?
It is hoped that those infected by tainted blood and their families will discover exactly who was responsible. But will criminal charges be brought? Several options are available to prosecutors.
Where those infected by contaminated blood have died, individuals identified as responsible may be charged with gross negligence manslaughter. Where the collective fault of an organisation can be identified, a charge of corporate manslaughter might be brought – but in cases where victims died before this crime was introduced via the Corporate Manslaughter and Homicide Act 2007, prosecution under the old common law offence of corporate manslaughter is unlikely to succeed.
For injuries short of death, individuals who recklessly supplied the contaminated blood could be prosecuted for grievous bodily harm under Section 20 of the Offences Against the Person Act 1861. Proving that individuals were grossly negligent or reckless – and that this negligence or recklessness caused the death of the victim – will be hard. Proving the Department of Health guilty of corporate manslaughter might arguably be easier, although prosecutors would also need to demonstrate how the department’s policies or practices directly led to the contamination of blood products, causing the victims’ injuries and deaths.
There have been instances where doctors have been charged with gross negligence manslaughter following the death of patients through negligence, and one instance of a prosecution of an NHS Trust for corporate manslaughter, which was unsuccessful.
Due to the time that has passed and the complexity of the law, it is quite possible that the courts will be unable to hold anyone criminally accountable. But the decision to allow victims to begin proceedings against the Government goes some way towards providing victims some level of justice. If a rigorous, victim-centred inquiry is also conducted, they and the public may at least find some closure in their search for the truth of the failings that scarred thousands of people’s lives.
Handled properly, this inquiry will at least send the message that such professional and institutional failings are unacceptable – and the Government’s admission of liability would be a first step toward providing victims with the justice they have sought for so long.
Melinee Kazarian is a lecturer in healthcare law, at the University of Southampton. This article first appeared on The Conversation (theconversation.com)
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments