How pulse oximeters have made thousands of operations safer
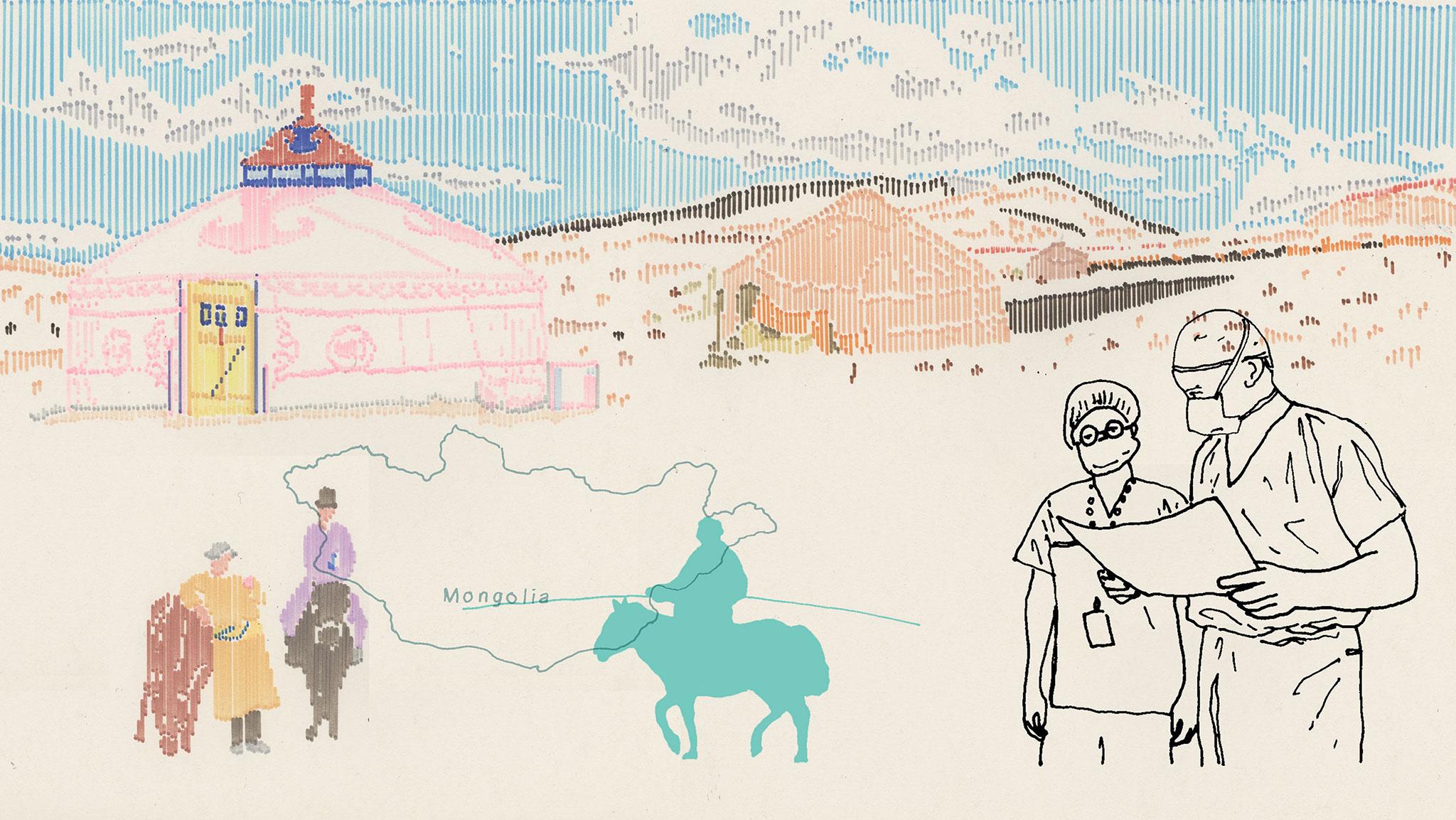
Millions each year die or are left disabled following surgical complications when one simple piece of kit could have saved them. Jane Feinmann discovers how it has helped transform medicine in Mongolia

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Gundegmaa Tumurbaatar glimpsed her son only for an instant as he was carried into the ageing Soviet-built hospital where she works. It was one of the first fine days after the gruelling Mongolian winter, and she had left Gunbileg, aged three, and his older brother playing outside, telling them to be careful. Now, he was moaning in pain and covered from head to toe in filth and blood. A passer-by had brought Gunbileg to the hospital after seeing the two boys trying to jump over an open manhole above a sewer – watching in horror as the younger boy had fallen into the jagged pit on his abdomen. By the time Gundegmaa saw him, he was in shock, his belly frighteningly distended, an internal haemorrhage putting him at imminent risk of cardiac arrest.
She learned the details of his injuries later: his spleen, the delicate fist-sized organ that sits just below the ribs and acts as a blood filter as part of the immune system, was ruptured. “His tummy must have caught on something sharp inside the hole in the ground,” she says. But she didn’t need to be told how serious this was. As soon as she saw him, Gundegmaa, a midwife at the hospital, knew that this was a potentially fatal internal injury. Suddenly, the life she and her husband, Batsaikhan Batzorig, had created with such effort looked about to turn to dust.
Gundegmaa and Batsaikhan were both born in the small town of Ondorkhaan in Khentii Province – one of the coldest spots on the Mongolian Steppe and 330km of often deeply pitted road from the capital city, Ulan Bator. They had married soon after leaving school, and their first child was born 12 years ago.
Back then it was a grim time in Mongolia, which was still in the grip of the desperate poverty that hit when 70 years of Soviet influence ended in the early 1990s. Russian forces had withdrawn from the country, taking with them the loans that had kept Mongolia afloat. It was fortunate that there were, and still are, hundreds of thousands of nomads in the country, around a quarter of the population. With their livestock – 25 million cows, horses, sheep and goats – at least people didn’t go hungry.
But the couple worked hard to build a life together. First, Gundegmaa enrolled at the nursing school in Ulan Bator that had been established under the Soviet “Semashko” healthcare system. Her husband remained at home with their baby, then three years later they swapped roles around, so that by 2010 both had jobs with the local hospital. He was a senior nurse; she was a midwife.
Their home town was also on a roll, it being the capital of the province where the 12th-century Mongol warrior Chinggis Khaan (Genghis Khan) is thought to have been born. During the Soviet era, Mongolians were forbidden even to utter the name of the man they now regard as their national hero. But in 2013, the town known as Ondorkhaan was grandly renamed Chinggis City by an act of parliament. Gundegmaa and her family could visit a new museum featuring a replica of the great leader’s ger, the traditional tent, made of white felt, of this nomadic people. The town’s playgrounds, as throughout Mongolia, have figures of children (of both sexes) engaged in the “three manly sports” – horse riding, wrestling and archery – that Chinggis Khaan considered essential daily activities for his warriors.
Just two weeks before Gunbileg’s accident, the family had moved into their first proper home, a flat in one of the new high-rise blocks.
On duty the day of the accident was Dr Mendbayar Lkhamsuren, an experienced surgeon with more than 4,200 operations under his belt since he started working at the hospital in 2000 – including, crucially, four previous cases involving a ruptured spleen. Through his training in safe surgery, Mendbayar has a genuine humility about the work he undertakes. “When I wake up in the morning, I reflect on the fact that I’m only human and that I’m just as capable of making mistakes as anyone else,” he tells me.
Mendbayar and his surgical team worked fast to remove the spleen and stem the bleeding, and Gunbileg survived. Now aged four, he needs to have all his jabs: without his spleen, he’s at increased risk of infectious diseases such as pneumonia and flu. But he is brimming with health and optimism, and has a passionate attachment to “my doctor Mende”. When I meet him in the antenatal department of the hospital, keeping close to his mother, he lifts up his long white jacket, just like his hero’s, which covers a prominent scar on his tummy.
A major contributory factor to his survival is a very bright idea that is changing emergency healthcare for people living in low- and middle-income countries.
As Gunbileg was carried into the emergency room in May last year, a nurse placed on his finger a small peg-like device attached by a wire to a battered-looking yellow monitor the size of a mobile phone. “Don’t be taken in by appearances,” the hospital’s anaesthetist says as she sees me squinting to inspect it during my visit last October. “That device has been used every single day for the past four years. It’s saved hundreds of lives. And it’s still going strong.”
The device is a pulse oximeter. Invented by Japanese scientists in the early 1970s, this non-invasive device, which attaches via a clip to the top of the patient’s finger, accurately measures blood oxygen saturation – the percentage of haemoglobin in the blood that is oxygenated – and displays the figure on the monitor along with the patient’s pulse rate. The device’s audible beep reassures the team that all is well, with the pitch dropping if there’s a problem, allowing the anaesthetist to “hear” any changes in oxygen saturation levels.
In high-income countries today, pulse oximeters are part of the furniture in recovery rooms, ambulances, accident and emergency departments and many hospital wards – wherever patients’ symptoms are serious and unpredictable. Its most important role, however, remains where it first began: in the operating theatre. “Oximetry is a key component in the revolution in anaesthesia care that has brought down the death rate from anaesthesia by over 95 per cent in a generation,” says Dr Atul Gawande, the Boston surgeon, bestselling author and New Yorker magazine writer. In the early 1970s, one in 10,000 people per anaesthetic administered died while under the gas in the USA: thousands of people were dying every year. By the 1990s, when pulse oximetry was routinely used, that was closer to the current figure of less than one in 100,000.

Yet the benefits of pulse oximetry have failed to spread throughout the world. According to a survey carried out in 2010, two decades after pulse oximetry became routine in affluent countries, more than 77,000 operating theatres in low- and middle-income countries were carrying out surgery without a pulse oximeter .
Meanwhile, the rate of surgery in these countries has been increasing. According to the World Health Organisation (WHO), the annual number of operations globally increased from 226 million in 2004 to an estimated 313 million in 2012, with much of this being down to the 115 per cent increase in the surgical rate in low-resource countries and the 69 per cent increase in very-low-resource countries. And rightly so, says Gawande. “Of course this rate of surgery is needed,” he says. “More people die every year from conditions that can be effectively treated with surgery than from HIV, malaria and tuberculosis combined. And surgery is essential for reducing maternal mortality and deaths from road traffic accidents.”
The problem is that while the rate of surgery is increasing, so is the rate of those damaged by surgery. Research published in The Lancet in 2009 shows that more than seven million people are left dead or disabled from complications due to unsafe surgery every year – with the risk of complications and deaths from essential operations up to 1,000 times higher in low-resource settings.
All but the newest recruits to the Mongolian anaesthesia community understand the background to these statistics. Dr Unurzaya Lkhagvajav, a former president of the Mongolian Society of Anesthesiologists, qualified as an anaesthetist in 1980 and reckons she has provided anaesthesia for 30,000 operations. The equipment she had available to keep a patient safe during most of these operations was a stethoscope, a watch with a second hand, and a pencil. “The only way to know if a patient’s blood was oxygenated was to take the patient’s pulse throughout the operation and check the colour of the fingernails: if they were pink, the patient was in good health,” she recalls. “It was exhausting work. And once the operation was over, the need to monitor blood oxygen levels is just as important. The only way to check for post-surgical complications was to sit with the patient all night. And of course that wasn’t always possible, not when you had a long shift the next day.”
In 2008 Gawande, at the request of the WHO, led a group of expert nurses, anaesthetists and surgeons to create the Surgical Safety Checklist. Essentially, it is a communications framework designed to eliminate human error in the operating theatre in the same way as the aviation industry has made flying safe for passengers. But alongside behavioural change to ensure effective teamwork and, for instance, that appropriate bloods and equipment are easily accessible and antibiotics administered, there’s a single piece of kit, the pulse oximeter, that is mandated by the checklist. Without it, the WHO decided, surgery is simply unsafe.
In 2011, with the support of prominent medical institutions, Gawande helped to found the charity Lifebox to make safe surgery a reality throughout the world. “We started by doing work that reduced the cost of robust, hospital-grade pulse oximeters for low-income countries by over 80 per cent to just $250,” he explains. The Lifebox oximeter can withstand extreme heat and cold and the battery is functional for at least 12 hours. Crucially, it is also tough, and can be dropped from table height without breaking. “It’s not going to break down soon after arrival, a serious problem with medical equipment in low-resource countries,” says Gawande.
Studies suggest that the WHO checklist, when used correctly with pulse oximetry, reduces complications and mortality by 30 per cent. By providing pulse oximeters in low-resource settings, Lifebox estimates that it has contributed to making surgery safer for 10m patients. Through donations, Lifebox has distributed nearly 15,000 oximeters to hospitals in settings where even the cheapest and most fragile oximeter is unaffordable. But it’s much more than this, Gawande says. “If all we were doing was parachuting in a bunch of pulse oximeters, we wouldn’t have such a tremendous impact.” Instead, through a volunteer network of anaesthetists from high-income countries, Lifebox has supplied thousands of anaesthesia providers in low-income countries with safety skills training. “Once you introduce the device and safety training into the riskiest part of the hospital system, you begin to build confidence that there are professional values at work aimed at generating better, safer care,” Gawande explains. “It gives clinicians confidence that they can take on more difficult cases. And people begin to believe that turning to hospitals when you are in desperate trouble is safe, that these are places you want to go.”
Dr Ganbold Lundeg was surprised when he first read the Bible – and not pleasantly. It was 1993, a low point in Mongolian history, when post-Soviet medicine, like the country itself, was floundering. Ganbold, a lecturer in anaesthesia at the Health Sciences University of Mongolia, wasn’t alone in wondering whether the Bible, much promoted by a visiting surgeon and missionary from Arkansas, USA, Dr Albert “Buck” H Rusher, might offer an answer. So he decided to learn English in order to read it.
The American’s Bible classes were a hit with the Mongolian medical community. “Some doctors were converted to Christianity without reading the Bible,” recalls Ganbold. “I wanted to read it first.” He enrolled at an international school, attending the one English-language course in the whole of Mongolia at the time. “I’d heard so much about the Bible,” he recalls. But the text, particularly the Old Testament, was unimpressive, “just like the fairy stories we heard as children”.
Yet he has never regarded as wasted the time he devoted to reading how Moses led his people through the Red Sea. Learning English gave him access to English-language medical journals, to which he was able to subscribe with the support of the missionary. “Even in the 1990s, these journals were regarded as subversive – they always arrived opened. I once had a visit from a member of the KGB who wanted to know why I was receiving them.”
Most importantly, he says, speaking English enabled him to make a personal connection that has undoubtedly helped to save hundreds, perhaps thousands of lives. In 1999, a Melbourne-based anaesthesiologist, Dr David Pescod, arrived in Ulan Bator to attend a medical conference. On that first visit, Pescod survived on mutton fat and vodka and spent two weeks listening to lectures in Mongolian interspersed with electricity cuts, all in -20C temperatures. The only other fluent English speaker present was Ganbold, who asked Pescod to return to deliver a lecture the following year. Pescod kept going back, forging links there together with a group of Australian colleagues, and what he learned about anaesthetic practices in Mongolia surprised him.
Mongolian surgical training and practice, he realised, were based on outdated, frankly dangerous 40-year-old Russian texts, with patients being given inappropriate anaesthetic drugs and at insufficient doses. Pescod settled down to write a series of anaesthesia textbooks designed specifically for Mongolian hospitals.
In 2004, Ganbold’s department, supported by the Australian team, started to implement the WHO’s Emergency and Essential Surgical Care programme, aimed at strengthening surgical services outside the capital city. “Many people think that surgery is something very special that cannot be delivered in a developing country or in a rural area,” he says. “But when we build up safe conditions, educate people and train them appropriately, then doctors and nurses can deliver safe surgery in a very small hospital anywhere in Mongolia.”
The recent safe surgery developments have built on this innovation. In 2011, the WHO Surgical Safety Checklist was made mandatory by the Mongolian health department. By 2012, funding from Australian and New Zealand anaesthetists had paid for 116 Lifebox pulse oximeters: 64 in Ulan Bator, three in Chinggis City and the others distributed throughout the country. The oximeters themselves have been physically delivered by Lifebox, which also provides teaching materials for a one-day course on pulse oximetry that is now incorporated into a week of training on safe anaesthesia that Pescod and his team continue to provide each year in Ulan Bator and throughout Mongolia.
Lifebox pulse oximeters have been handed out to surgical teams at “inter-soum” hospitals, the large district hospitals such as the one in Chinggis City, as well as at smaller soum (township) hospitals, enabling local staff to respond to emergencies. At one level, it means that around 200 people a year with acute appendicitis are treated in Khentii Province instead of having to travel to Ulan Bator – the only location able to carry out appendectomies until four years ago. At the other extreme, emergency patients like Gunbileg receive urgent life-saving surgery.
In January 2014, Ganbold became one of 25 clinical experts advising the Lancet Commission on Global Surgery – “the proudest achievement in my professional career” – with its aspiration to make safe surgery and anaesthesia a human right available to all. Mongolia is now cited by the Lancet Commission as a potential model in promoting safe surgery and anaesthesia for other medium-sized countries such as Myanmar and Laos, and even for India and China.
Ganbold’s great ambition is to open 20 hospitals with functioning operating theatres by 2020, by building up services in strategically located provincial clinics. If that means going cap in hand to wealthy countries and organisations, that’s what he does. In Ulan Bator, we visit the UK ambassador to Mongolia, and Ganbold explains to her how the UK government could provide assistance with the minimum of funding. The UK firm Diamedica has pioneered the production of basic anaesthesia machines that can be used virtually anywhere without electricity or even medical gases. Ganbold urges the ambassador to consider funding such machines for hospitals in remote Mongolia. She agrees to consider the idea.
It’s this persistence in seeking out and achieving the best that keeps Pescod coming back to Mongolia, he says. “Unlike other countries where I have lectured, eventually everything we bring to Mongolian anaesthetists has been engaged and usually improved,” he tells me.
Dr Bilguun Unurbileg, a senior lecturer in anaesthesiology at the Health Sciences University of Mongolia and Ganbold’s number two, says that’s down to their nomadic ancestry. “Mongolians are hard-wired to reach out for new ideas. That’s the result of centuries of living in the middle of nowhere, entirely reliant on yourself to care for your family. It’s how we survive.”
Two thousand miles south of Ulan Bator, Assam in north-east India has twice the country’s already high average maternal mortality rate: there are around 300 deaths per 100,000 pregnancies in Assam, compared with 174 in India as a whole and just nine in the UK. Three-quarters of these deaths occur among the 800,000-strong female workforce employed in Assam’s tea gardens, where the high number of perinatal emergencies is the result of the harsh conditions of the working day. Even when women and their babies do get successful surgery in the nearest properly equipped hospital, post-operative care remains hazardous, partly because of the lack of pulse oximetry in recovery wards.
“Healthcare for mothers working in tea gardens is pathetic,” says Dr Surajit Giri, a consultant anaesthetist and critical care physician based at Demow Community Health Centre near Sivasagar, northern Assam. He is employed by the Indian government as part of its recently established National Rural Health Mission. But he’s well aware of the deficiencies of the service. Demow is the only clinic providing care for seven tea gardens – and has only one operating theatre, with basic obstetric intensive care facilities.
Last October, Giri helped to organise (and attended) a “Train the Trainers” workshop in Dibrugarh, organised by Lifebox, focusing on the benefits of pulse oximetry in post-operative care – an area local practitioners had identified as being one where they most needed support. UK consultant anaesthetist Dr Neeraj Bhardwaj talked 68 local anaesthetists through a one-day “Safer Anaesthesia” workshop. And at the end of the day, each practitioner was able to go back to work with their own new Lifebox pulse oximeter.
The day after receiving the Lifebox oximeter, Giri made it mandatory for nurses at the health centre to monitor oxygen saturation levels in newborn babies, using the neonatal probe that comes with the adult oximeter for an extra $25. Already, he says, healthcare is safer. “That day, a baby was delivered that was shown by the probe to have just 58 per cent oxygen saturation. The nurse immediately shouted for my help to resuscitate the baby, which I rushed to do – and it soon started crying healthily, maintaining oxygen concentration without assistance. Without the oximeter, that would not have happened. If five minutes had gone by before we took action, the baby would probably have survived, but with a disabling brain injury.”
The Dibrugarh course is the first event of a three-year initiative funded by the Stavros Niarchos Foundation that will eventually hand out 675 Lifebox pulse oximeters, with appropriate training, initially in three regions of India: Bihar, Odisha and Assam. It’s the start of a journey to transform surgery in a country where currently 7,000 out of 155,000 operating theatres lack pulse oximetry.
“Of course Lifebox pulse oximeters increase the safety of patients,” says Giri. “But they also increase the security and confidence of anaesthetists to join rural services, which they haven’t done before because of lack of technology and poor infrastructure.”
Ankhbaatar (not her real name) was 38 weeks pregnant when, lifting a heavy load while setting up camp in her felt-walled ger, she felt a sudden sharp pain in her abdomen. It was September 2015 and she knew straight away that her baby was at risk.
The nomad family’s ger was pitched in Khovd Province in western Mongolia. It’s a natural paradise: a vast area of snow-covered peaks, rocky deserts and salt lakes that is an adventure playground for tourists in the summer and a favoured location for Mongolia’s nomads to graze their herds of sheep, goats and yaks.
Ankhbaatar used her mobile phone to summon the rural soum doctor from a small surgery a 20km off-road drive away. He examined her, and confirmed that she had suffered a placental abruption, the pressure from the load she was carrying almost certainly causing a swathe of blood vessels that feed the fetus to detach from the wall of the uterus.
“The rural doctor reported that the fetus was distressed and that it was out of the question for the mother to travel to us,” recalls Dr Nansalmaa, an obstetrician based in the main hospital in the city of Khovd. So the obstetric team, Nansalmaa, an anaesthetist and a neonatologist went to Ankhbaatar’s ger, together with the basic equipment needed to carry out an emergency caesarean section, including an oxygen concentrator and suction machine, an operating lamp, a Honda electricity generator and, perhaps most importantly, a pulse oximeter.
Within hours of an incident that until recently would have consigned Ankhbaatar and her baby to becoming yet another obstetric fatality, both mother and baby survived thanks to safe spinal anaesthesia followed by a caesarean section.
Ger surgery is rare. But when necessary, it happens without fuss. For nomadic patients, that instils confidence: not just in the healthcare system, but also in their chosen traditional lifestyle. That’s what I discover when I call on Tumurdavaa Gursed in the ger that was the location for her emergency surgery eight years ago, when she was close to death due to a ruptured ectopic pregnancy. She too was unable to travel, and would have died had the emergency surgical team not already been in operation and ready to travel through the night to carry out the emergency operation – albeit without a pulse oximeter – at first dawn.
I sit on the low bench used for the operation, reflecting on the commitment of the team back then – carrying out a two-hour operation in a roasting hot ger, the anaesthetist bent almost double throughout to monitor his patient.
Tumurdavaa, serving boiled horse with blood pudding and potatoes along with fresh cream and biscuits, is silent as we eat. I take it for shyness at first, but then realise it’s simply a lack of interest in small talk. When I ask her about her brush with death, she talks at length, eloquent in paying tribute not only to the medical team but also to the impact of the policy of safe surgery on nomadic life. “I’m so joyful and reassured,” she tells me, “that I can continue living blissfully beside my animals.”
This article was first published by Wellcome on Mosaic and is republished here under a Creative Commons licence
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments