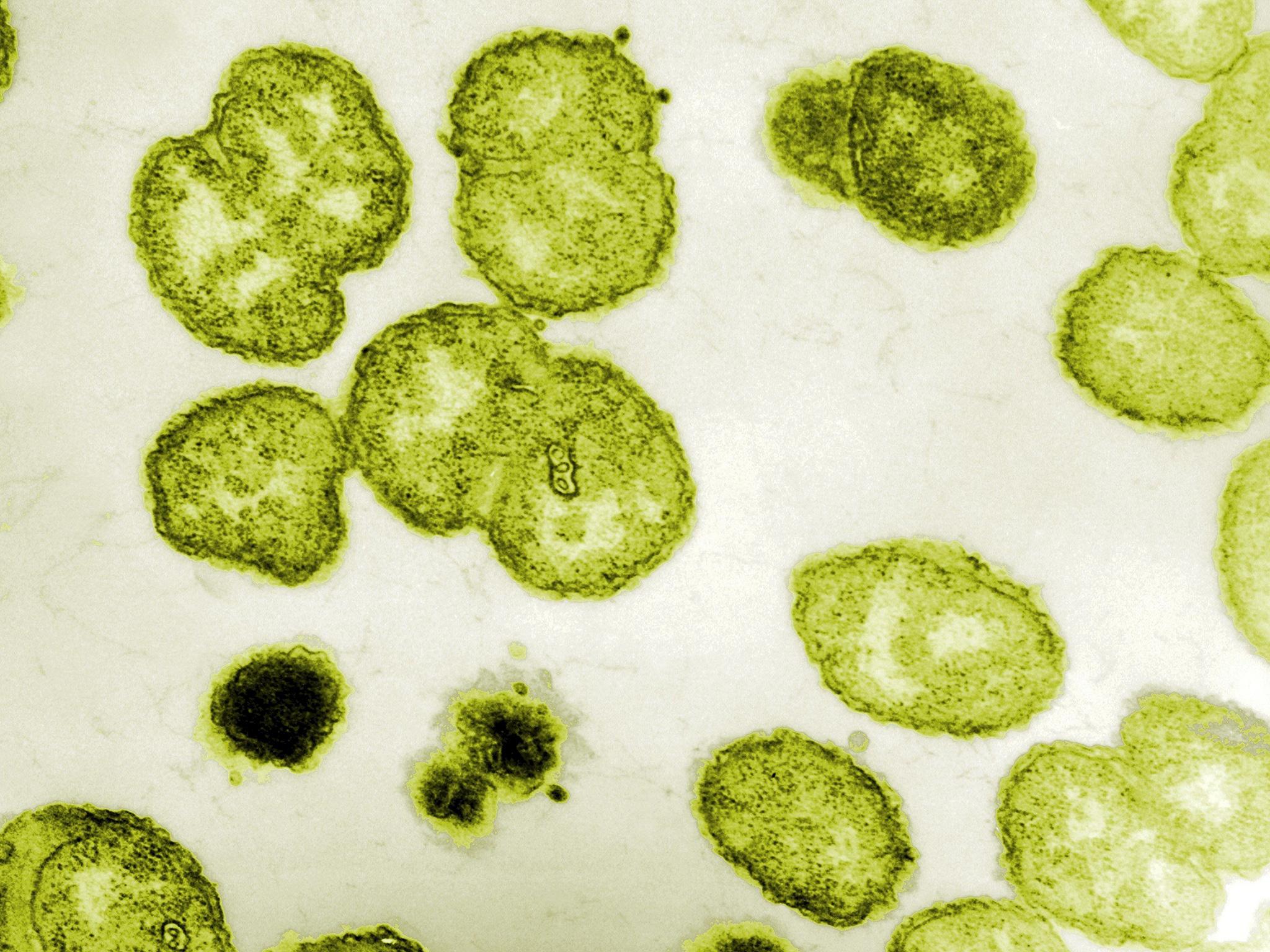
Gonorrhea antibiotics rendered ineffective by STI's 'high levels of resistance', WHO warns
The sexually transmitted disease could become untreatable with 'serious sexual and reproductive health consequences', World Health Organisation says
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.An entire class of antibiotics should not be used to treat one of the main sexually transmitted diseases, gonorrhoea, because it has developed “widespread, high levels of resistance”, the World Health Organisation has warned.
More commonly known as ‘the clap’, gonorrhoea typically causes pain when urinating and produces a thick green or yellow discharge, but also sometimes causes few noticeable symptoms.
However, if untreated, it can lead to infertility and also cause blindness to the unborn child of an infected mother.
Once it was cured simply with one dose of antibiotic, but the bacteria that causes the disease has been evolving to develop resistance to the drugs.
The WHO said the rapid rise of resistance in gonorrhoea was “raising concerns about the eventual development of untreatable gonococcal infections with serious sexual and reproductive health consequences”, repeating a warning issued by other experts last year.
In a statement, the WHO said quinolones, a broad-spectrum antibiotic normally reserved to treat resistant strains of disease, were no longer recommended for use against gonorrhoea.
“Antimicrobial resistance has appeared and expanded with every release of new classes of antibiotics for the treatment of gonorrhoea,” it said.
“Because of widespread resistance, older and cheaper antibiotics have lost their effectiveness in treatment of the infection.”
The WHO advised countries’ health authorities to monitor resistant strains of gonorrhoea within their populations.
“The new guideline calls on health authorities to advise doctors to prescribe whichever antibiotic would be most effective, based on local resistance patterns,” the WHO statement said.
“The new WHO guidelines do not recommend quinolones for the treatment of gonorrhoea due to widespread, high levels of resistance.”
Quinolones are not the first-choice antibiotic for gonorrhoea in the UK, but currently can be prescribed, for example if the patient is allergic to the usual drug.
This is usually done in combination with another antibiotic and after testing to establish the strain of gonorrhoea is not resistant.
Antibiotic resistance is growing across a broad range of diseases, to the extent there are fears that antibiotics will eventually become useless, returning medicine to the time when a simple scratch in the garden could be fatal.
Major operations like transplants would also become impossible because the risk of infection would be so great.
Many experts see this as one of the biggest public health dangers facing the world.
In December last year, a superbug resistant to the antibiotic of “last resort”, colistin, was found in the UK in human cases and on three farms.
Earlier this year David Cameron warned there would be “catastrophic consequences” if the problem was not dealt with as he pledged the Government would halve drug-resistant infections by 2020.
And last month, leading experts called for an average limit of nine antibiotic doses per person a year in an attempt to stop the rise of superbugs.
Antibiotics have been used as growth agents in livestock, something experts warn is the perfect way to develop resistance as the regular, low doses damage but do not kill the bugs.
The EU outlawed this in 2006, but in some countries the use of antibiotics to supposedly treat disease in animals increased, leading to suspicions farmers were getting round the ban.
Another significant problem is antibiotics given to people with colds and flu. Both are viruses so are not affected by a drug designed to kill bacteria, but many patients demand them and some doctors relent.
NHS England declined to comment, saying treatment recommendations were "the domain of NICE", the National Institute for Health and Care Excellence, and the British Association for Sexual Health and HIV (BASHH).
A NICE spokesman said: "Unfortunately NICE has not issued guidance on quinolones or treatments for gonorrhoea."
According to "advice" published on NICE's website: "The prescribing of quinolones (for example, ciprofloxacin and ofloxacin) in general practice is also a cause for concern.
"Resistance to quinolones has increased at a considerable rate (for example, quinolone-resistant Neisseria gonorrhoeae) and is usually high level, affecting all the quinolones.
"Public Health England guidance on managing common infections recommends that quinolones are used as first-line treatment only for acute pyelonephritis, acute prostatitis, epididymitis and pelvic inflammatory disease. It states that they should be used in lower respiratory tract infections only when there is proven resistance to other antibiotics."
According to the BASHH website, the antibiotic ceftriaxone, not one of the quinolones, is normally prescribed for gonorrhoea.
It notes that the disease has "progressively exhibited reduced sensitivity and resistance to many classes of antimicrobials", including quinolones.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments