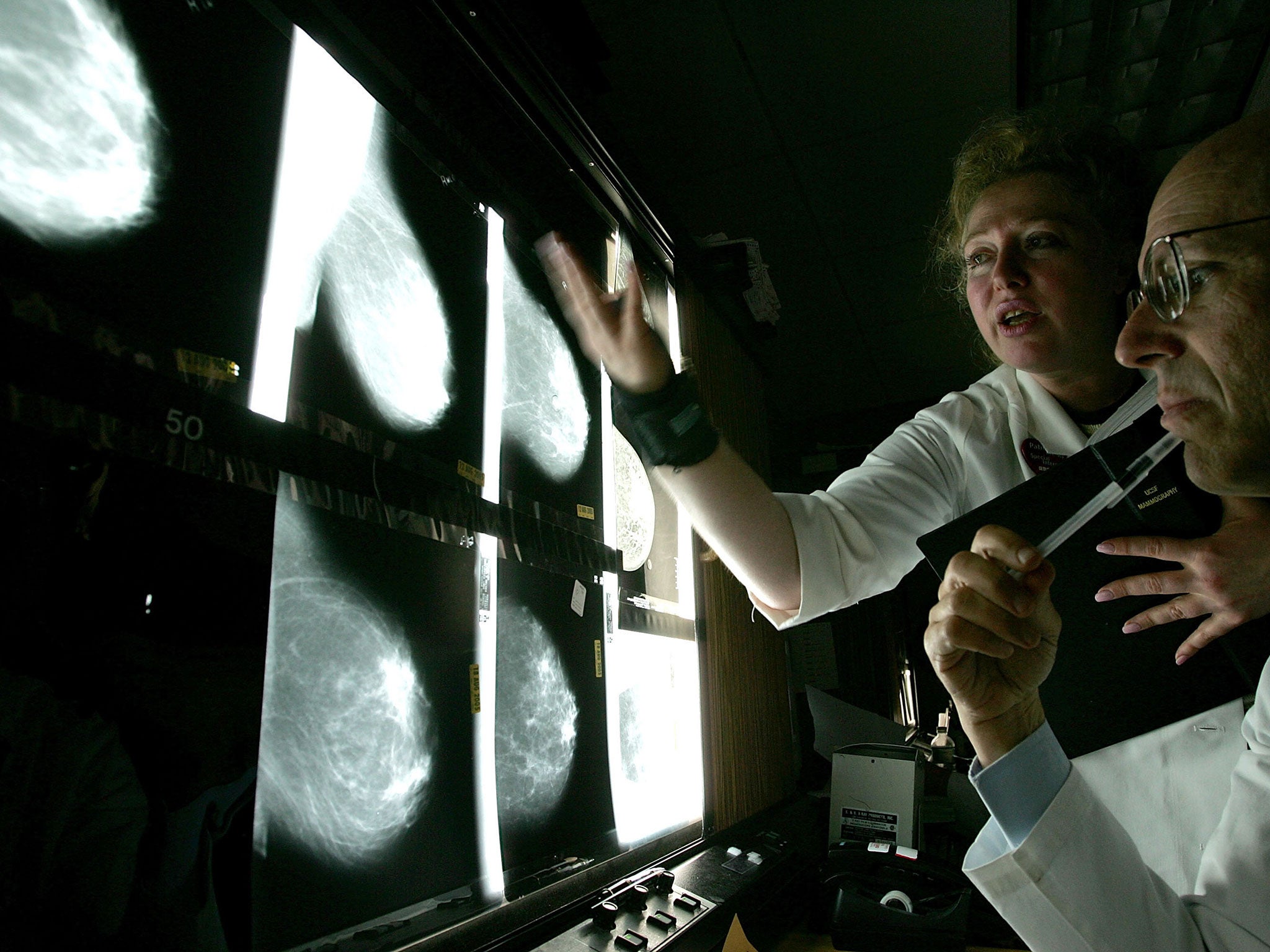
Breast cancer: Preventative double mastectomies 'do not improve quality of life'
There has been a sharp increase in double mastectomies in recent years
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.For years, doctors and researchers have been concerned about a surprising trend: More and more women with early-stage cancer in one breast were choosing to have double mastectomies to reduce the risk of cancer in the other.
Many of the patients said they thought an aggressive approach would help their quality of life by lessening their worries about future cancer and making them more comfortable with their bodies.
But new evidence released Monday shows that the surgery doesn't improve peace of mind or quality of life very much.
Researchers at the Duke Cancer Institute surveyed thousands of women who had cancer in a single breast and underwent single and double mastectomies. They wanted to see whether the double-mastectomy patients were less anxious, more satisfied with their physical appearance and more confident in their sexuality. They found that the double-mastectomy group had only a slight edge — primarily among women who had undergone breast reconstruction.
“What this shows is removing a healthy organ doesn't improve quality of life as much as women think that it might,” said senior author Shelley Hwang, the institute's chief of breast surgery. She said that women continued to have anxiety about cancer, regardless of which surgery they had.
Studies over the past decade have shown a sharp increase in the use of double mastectomies — contralateral prophylactic mastectomies, or CPMs — to treat breast cancer in a single breast not caused by an inherited gene mutation. More than 11 percent of women had such surgeries in 2011, compared to just 1.9 percent in 1998, according to a 2014 study.
But “unless a woman has a gene mutation that places her at significantly increased risk of a new cancer in the other breast, CPM doesn’t prolong life, and our study shows that it doesn’t make for a notably better quality of life,“ Hwang said.
“Breast surgeons as a community are very worried about women using this kind of surgery to alleviate anxiety,” she added. “Surgery is meant to cure a biological problem, not make people feel less anxious.”
Many women with cancer in one breast overestimate their risk of developing cancer in the other breast, which is actually low. Some doctors aren't adequately explaining the risks involved, she said.
“Maybe we need to educate women better,” she said, adding that double mastectomies carry their own risks, including possible numbness across the chest wall, chronic pain and repeated infections.
To conduct the study, Hwang and other researchers surveyed 4,000 women who participate in the Army of Women, an organization that provides volunteers to researchers conducting breast-cancer research. All had undergone single or double mastectomies, and the researchers measured their physical and sexual well-being, as well as satisfaction in their appearance.
The Duke study, which was published online Monday in the Journal of Clinical Oncology, showed that women who had CPMs tended to be younger, with higher incomes and earlier-stage disease. The study also found that having breast reconstruction was the single most important factor in a better quality of life.
Hwang stressed that the research excluded women with a much higher cancer risk due to the presence of a genetic mutation, such as BRAC1 or 2. “That's a totally different situation,” she said.
The Duke study echoes the findings of a study presented last year at a conference of the American College of Surgeons. That study found that for younger women with early-stage, non-inherited cancer in one breast, a single mastectomy leads to a slightly higher quality of life and lower costs over the two decades, compared with CPMs.
The Washington Post
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments