The eye-feasting parasite that can get in through your contact lens
Lenses can be contaminated by exposure to water during swimming, using a hot tub, washing with tap water or as a result of poor personal hygiene. If untreated, an Acanthamoeba infection can lead to blindness

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
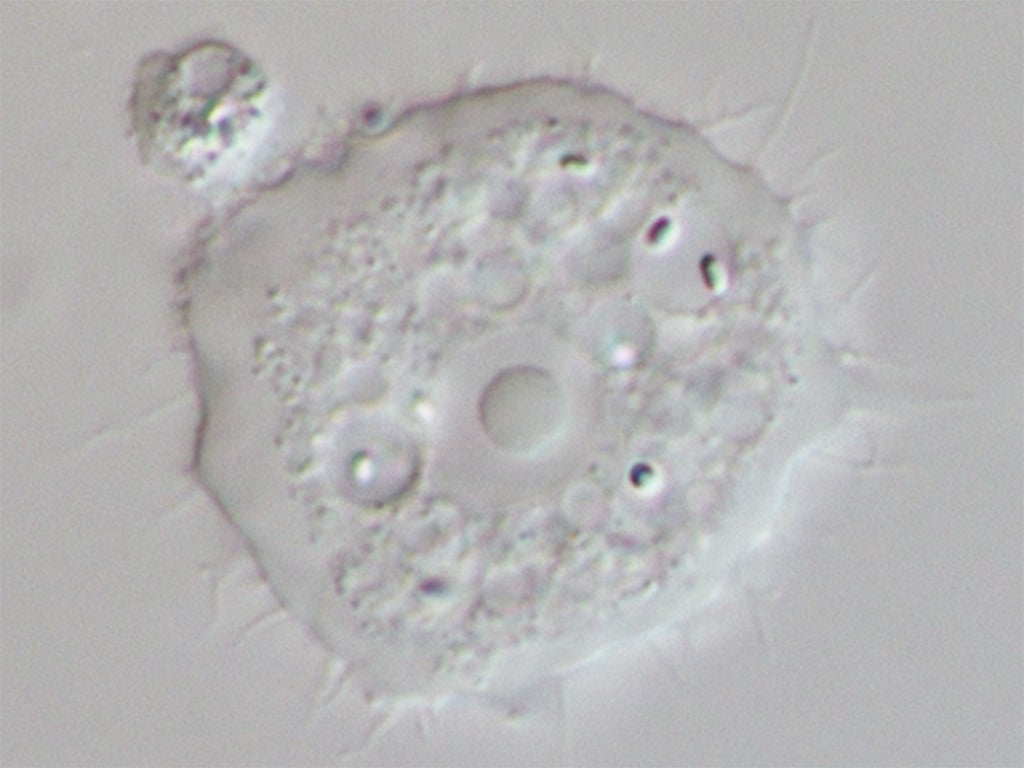
Your support makes all the difference.A recent eye infection suffered by 18-year-old Nottingham University student Jess Greaney is the kind of story that fills us with horror. Greaney had keratitis, an inflammation of the cornea, caused by Acanthamoeba castellanii, a parasite that was living and feasting on her eye.
A. castellanii is a ubiquitous organism, found in many eco-systems worldwide. It is able to survive in harsh environmental circumstances – even in some contact lens solutions – and this is not the first occurrence of A. castellanii appearing in the eye. Acanthamoeba keratitis (AK) is a neglected malady frequently associated with contact lens wear and it is thought Greaney caught the bug after splashing tap water on her contact lenses.
Not a great friend to have
Acanthamoeba infection of the cornea causes severe inflammation, intense pain and impaired vision, which is blinding if left untreated. Infection begins when the parasite is at its active feeding trophozoite stage and sticks to the corneal tissue before penetrating the lower stromal layer. The resulting opacity leads to less sharp vision and eventually blindness.
Even more worrying is that besides the painful progressive sight-threatening corneal disease, the parasite can cross the blood brain barrier and cause granulomatous amoebic encephalitis, a progressive disease of the central nervous system) that often results in death.
Greaney was lucky – if you can put it that way – because she was able to receive treatment. After a week her eye was red, painful and bulged, “it looked like a huge red golf ball,” she said. Treatments included clamping her eye open, keeping her awake, scraping off layers of tissue and repeated eye drops.
How does it get in?
Lenses can be contaminated by exposure to water during swimming, using a hot tub, washing with tap water or as a result of poor personal hygiene or inappropriate disinfection regimes, which can promote the growth of bacteria on lenses onto which amoebae in turn adhere and proliferate. In the case of Greaney it was suggested that the parasite was trapped between the eye and the lens before it burrowed.
As contact lenses continue to gain popularity (including for recreational purposes) the proportion of the population at increased risk of developing Acanthamoeba keratitis may rise.
Other Acanthamoeba infections
Acanthamoeba infections (not just in the eye) are being detected by clinicians with increasing frequency, especially as opportunistic infections in patients whose immune system is already compromised. This at-risk population is expanding as a result of increasing use of immune-suppressing therapies for cancer treatment and the global HIV/AIDS pandemic.
No vaccine is available, and the current drugs used to treat these inflammatory infections is largely insufficient, has undesirable side effects and doesn’t work well in the later chronic stage of infection. Treatment also requires the application of a mixture of drugs for prolonged periods, with mixed results. New drugs, either for this or for other neglected parasitic illnesses that afflict millions of people worldwide, are not being developed. The development of cheaper and more efficient, preferably A. castellanii-specific, chemotherapies would be highly advantageous.
Practice good hygiene
When it comes to contact lens wearers, there have been previous efforts looking at whether contact lens care solutions can counter against Acanthamoeba. Contact lenses treated with an antimicrobial peptide have also been developed and tested in human and rabbits, but more clinical trials are still needed before they can be worn by humans.
However, there are some cardinal rules for contact lens wearers: always wash your hands and follow all instructions in handling and storing contact lenses properly. Reusable lenses should be cleaned and disinfected with powerful lens disinfecting solutions every day. Contact lens wearers should also apply make-up only after lenses are put in to avoid contact with eyeliner or mascara and lens. These are some of the “golden rules” that contact lens wearers should stick to.
Millions of people use contact lenses to improve their vision and to enhance the ability to focus or to do activities unencumbered by glasses. And overall, the risk of Acanthamoeba keratitis – and other infections – is low with proper hygiene and care. In the very near future we might even see smart lenses that can monitor the body’s health conditions and measure glucose levels in the tear fluid of the eyes of diabetes patients. So don’t let the horror story lead you to ditch them just yet.
Hany Elsheikha is Associate Professor of Parasitology at University of Nottingham.
This article was originally published on The Conversation. Read the original article.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments