Worried about blood clots? Here’s what you need to know
Blood clots have always been around – but they’re often preventable and treatable. Liz Connor finds out more.
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Every 37 seconds, someone in the Western world dies from a venous thromboembolism (VTE), where a blood clot forms, most often in the deep veins of the leg, groin or arm.
While clotting is a normal process that can prevent us from losing too much blood when wounded, clots that don’t dissolve can be dangerous, and even life-threatening in some instances.
Blood clots have also become a talking point recently, after the MHRA launched investigations into a potential link between AstraZeneca’s Covid vaccine and a spate of blood clotting events.
To better understand why blood clots sometimes occur and whether you should be worried, we asked doctors to answer some of our most common questions…
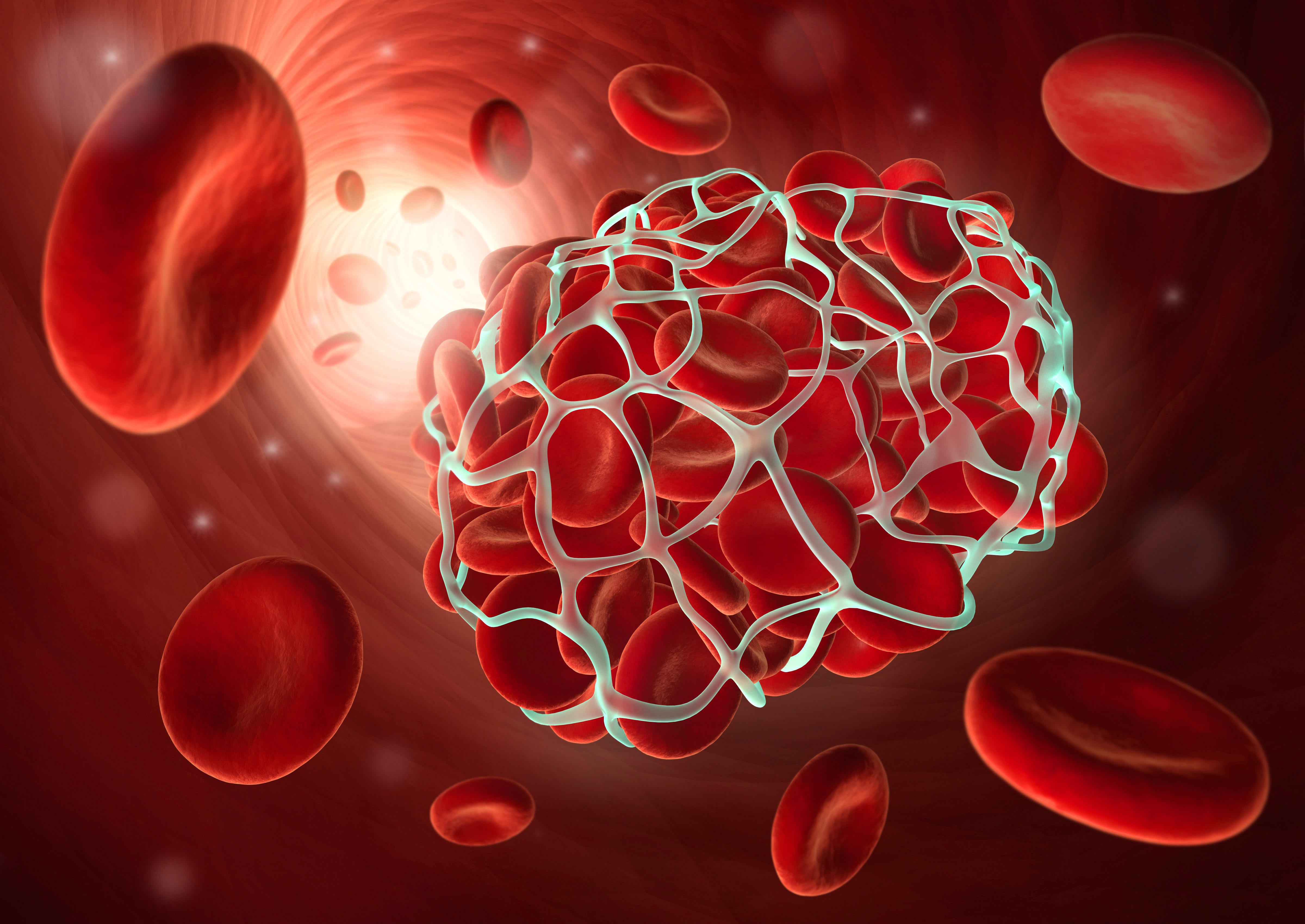
What are blood clots and why do they happen?
“Blood clot is a generic term for a thrombosis, which put simply, is an obstruction of a vessel (arterial or venous) by a build-up of platelets and a number of different blood products,” says Dr Emeka Okorocha (@doctor.emeka).
“If a particle of another product breaks off, it gets thicker and travels around the vessels, and may get stuck or create an obstruction. We call this an ’embolism’, which is also a form of blood clot.
“This process could be triggered by an injury, but in some cases blood clots occur inside vessels where there has been no obvious injury.”
What kinds of things put you at risk?
Blood clots can potentially affect anyone, although some lifestyle and genetic factors may put some people at higher risk.
“If you’re obese, bedridden after an operation, have very prominent varicose veins, are pregnant or are on an oestrogen oral contraceptive pill, then you may have an increased risk of blood clots,” says Dr Paul Ettlinger of London General Practice (thelondongeneralpractice.com).
They can also be associated with long lengths of time being inactive, and long-haul flights. According to National Blood Clot Alliance (stoptheclot.org), cancer, major surgery, the use of hormone therapy, smoking and being aged over 55 can also be risk factors. Genetic factors may also apply, so it’s important to know your family history.
What are the signs that you might have a blood clot?
It’s not always easy to spot whether you have a blood clot, because the symptoms are different depending on where you think you have it. But there can be some warning signs, especially for deep vein thrombosis (DVT).
“A DVT is commonly found in the leg, so look out for a painful swelling in the calf,” says Ettlinger. “This often happens after a period of immobility, which is why being on a long-haul flight or surgery can often cause an incident.
“Breathlessness and chest pain on breathing can be a sign that a clot has broken off and has entered the lung,” he adds (known as pulmonary embolism).
“But, of course, you can be breathless for lots of other reasons, even a common cold, so beware of any sudden acute onset,” says Ettlinger. This is especially important if you have a risk factor like taking the contraceptive pill, blood clots are in your family history, or if you’re pregnant.
“I’d also look at severe migraines too as a potential warning sign,” he adds.
How are blood clots treated?
“Medical experts often treat blood clots with blood thinning medication, such as anticoagulants,” explains Emeka. “We normally inject the medicine into the patient for a number of weeks, which basically thins the clot and reduces the more severe effects on the body.
“In more severe cases, we use percutaneous coronary intervention (aka a non-surgical angioplasty) to treat blood clots. If a blood clot is caused by something more serious and it has occluded in a vessel, then we can perform surgery. This involves a surgeon entering the vessel, stenting it and removing the clot completely.”
Should we be worried about the Covid-19 vaccine increasing your risk of blood clots?
“While there have been some reports of people suffering blood clots after receiving the AstraZeneca Covid-19 vaccine, the risk is minimal and the benefits outweigh the risk by a long way,” assures Emeka. “With a risk of only four in 1 million, people should not be worrying about developing blood clots following the vaccine and, on the whole, blood clots occur for a number of reasons, including lifestyle factors.”
What can you do to try and prevent blood clots?
As with many conditions, living a healthy lifestyle is one of the best preventative measures we can take. “It’s difficult to say whether you can completely prevent any clots from occurring, but if you keep your weight down, your cholesterol down, and control your blood sugar levels, then these can all contribute to reducing your risk,” says Emeka.
“One of the best ways to manage this is via a healthy diet and regular exercise. The NHS recommend at least 150 minutes of moderate-intensity activity a week, or 75 minutes of vigorous-intensity activity. If you’re not sure where to start, fitness apps like Freeletics (freeletics.com) can be incredibly beneficial.
“The app tailors workouts to you, your goals, and your fitness ability, so do not let being new to exercise be a barrier to starting, especially if you are worried about blood clots.”
Ettlinger suggests picking up some flight socks if you’re planning to travel when restrictions lift: “Support stockings, or flight socks, are a great way of reducing blood clots because they compress the veins in the legs and prevent blood pooling there and causing a clot.”
And Emeka adds: “Lastly, if you are taking the oral contraceptive pill or have blood clots in your family history, it’s advisable that you make sure you’re speaking to your doctor regularly about your risk.” While blood clots can be serious, they’re very treatable if caught in time.
If you have any concerns about your health and blood clot risk, speak with your own doctor or nurse.