The Independent's journalism is supported by our readers. When you purchase through links on our site, we may earn commission.
I was held hostage to the pill – quitting felt like jumping off a cliff
Sixty years after the introduction of the oral contraceptive pill, there is still scant evidence on what happens when you quit. For Sophie Gallagher a vacuum of knowledge kept her taking it for more than 12 years

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
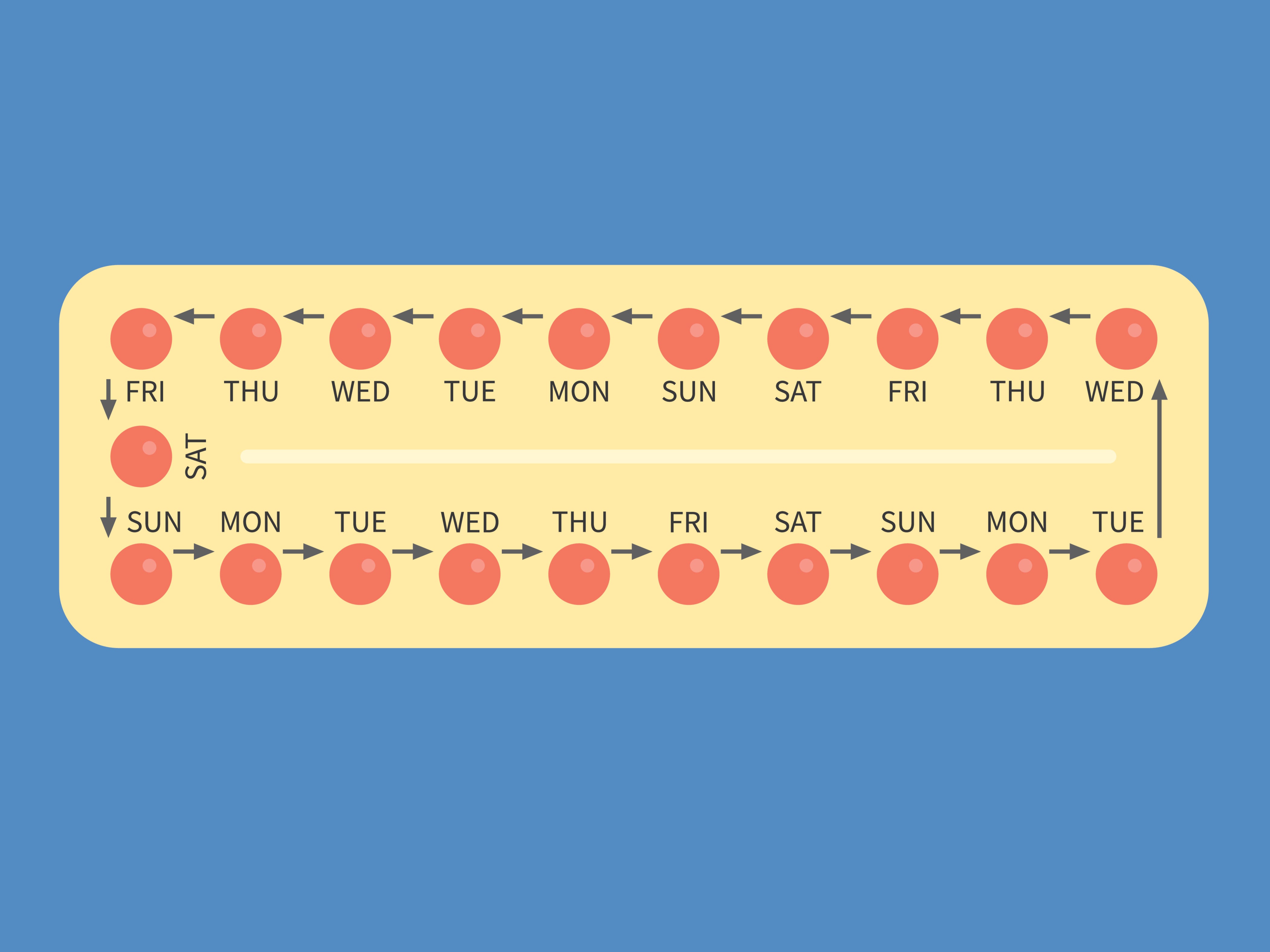
Your support makes all the difference.On the bad days I would take the box out of the bathroom cupboard, pop one from the packet and then just leave it on the side, eyeing it up over the course of an evening. I had wanted to stop taking the pill for a couple of years, but every time I came close I’d give into cowardice, fear of the unknown, a reluctance to rock the boat, or disrupt the cycle of artificial hormones my body had become so accustomed to.
Eventually I’d concede, pick up the little yellow pellet and gulp it down (a 12-year-long daily habit means you eventually get too lazy to require water). There was something about its smallness, its weightlessness, that simultaneously meant I could sneak it down my throat ignoring another day of defeat, but also felt insulting as such a tiny pill began to occupy more and more of my waking thoughts.
I’d spend hours Googling other people’s experiences, looking for what to expect on the other side. For years the pill had been a convenient liberation, but after a decade (the arbitrary upper time limit you’re warned of when starting, but upon probing seems more grey advice than black and white instruction) I became fearful of migraines; riding the waves of moods I wasn’t sure were my own; dealing with bad skin I couldn’t establish whether was being made better or worse by the pill; and resentful of the associated admin my partner could be totally oblivious to.
I asked more than one doctor, all unable to advise much beyond – if you don’t want a baby now keep taking it. But I didn’t want to keep taking it, I wanted out.
2021 marks 60 years since the pill was made available to all in the UK. On 4 December 1961, the health minister at the time, Enoch Powell, made the announcement many women had been waiting for, ushering in a new era of sexual, social and medical liberation. Five decades on, the problems that the pill can cause when taken are well documented: weight gain, loss of libido, depression and poor mental health – a 2018 BBC documentary highlighted the potential severity including suicidal thoughts in some. In the longer term, the pill slightly increases the risk of breast and cervical cancer (although lowers risk of other cancers), and marginally increases the risk of blood clots. Although not huge risks, a risk all the same.
On the whole women know this, we’re told about the risks by prescribing GPs, nurses and clinics while we’re taking it. But we still have a huge blindspot when it comes to another stage of our relationship with the pill: what happens when you stop taking it.
NHS data from December says there were 731,340 women in England using contraception in 2019-20 (based on data from sexual health clinics, but excluding GPs/pharmacies – the UN estimates 71 per cent of UK women aged 15-49 are using contraception). Of this number around 40 per cent are using a type of pill, making it the most popular method (the next highest is condoms). But this number has fallen from 2014/15 when it stood at 45 per cent as experts see greater numbers switching from the pill to long-acting reversible contraceptives like the coil.
Despite increasing data on pill uptake and the side effects while on it, there is still scant evidence on those who quit – about why they do and what happens when they go cold turkey. Will there be hormonal problems? Bad skin? Fluctuating weight? Loss of sex drive or changes in mood? For me, a snap decision made at the age of 17 to go on the pill wasn’t something I anticipated suffering the consequences of 13 years later – I thought I’d be an adult by then, who understood her body and the pill. Or at the very least I'd be given fair warning if I was signing an unwritten contract for future consequences down the line.

On the NHS website there is an entire multi-page contraception guide, but the brief section (269 words to be precise) on coming off the pill is dedicated to getting pregnant and the return of periods, implying that this is the primary, if not only reason, why someone might stop. And women's only concern. But a 1998 study (data is sparse) from the USA suggests this does not tally with reality, with nearly half (46 per cent) of women ditching it because of side effects compared to just a fifth (23 per cent) having no continuing need.
The Lowdown, a self-described “TripAdvisor for contraception”, which has gathered data on 3,500 UK users, found 78 per cent had experienced unwanted side effects, while 51 per cent said the pill negatively impacted their emotions and caused them to reconsider a future on it. Clearly, it is not always women looking to get pregnant who ditch it, and yet official information on what to expect is lacking. Instead, there are plenty of forums, YouTube videos, and tabloid headlines to fill the gap. On Reddit, women try to crowdsource information about what to expect.
Although this is not a new issue, it has been thrown into the spotlight once again during the pandemic as more than a third (36 per cent) of women have suddenly not known how to access their pill, according to research by MSI Reproductive Choices. The findings detailed that 35 per cent of women had experienced worse service, one in seven were unable to get an appointment, and one in 10 said that their clinic had closed due to Covid. Whether women choose to stop, or are forced by circumstance, how do they know what hormonal limbo awaits them on the other side?
I have developed Stockholm Syndrome with the pill - what if it is actually making everything better?
It’s been over 16 years since Stacey Benson, 31, from Herefordshire, first started taking the pill. At 14 she had such terrible acne that her mum took her to the GP, where she was prescribed the combined pill Dianette. Within two months her skin had totally cleared up. Over the years there were some mild side effects – headaches mainly, occasionally bad enough to require lying in a dark room – but for Benson it was a price worth paying to avoid acne.
Now, a 31-year-old living in Sydney, Australia, Benson feels differently. Granted, she still dreads waking up and seeing a pimple in the mirror – “I am quickly reminded of how insecure I felt” – but is beginning to wonder whether taking the pill is worth it for clear skin. When she really thinks about it, Benson has been weighing up this internal dilemma since the age of 23. But it’s easier to just keep taking it, another packet, another month, another year. Maintain the status quo.
Benson estimates she has tried stopping the pill more than 50 times: she has trawled the internet for advice, has listened to audiobooks, podcasts, any nugget of information she can find. On the first attempt it sent her skin into a downward hormonal spiral, which became so crippling it stopped her socialising. She couldn’t stick with it and rejoined the contraception carousel in a bid to reverse the effects.
Alice Pelton, who launched The Lowdown after her own bad experience with the pill and feeling there was a "big lack of useful data", tells The Independent that having spoken to hundreds of women, concerns about post-pill issues like breakouts or more painful bleeding, are among the most common. “Especially when it comes to skin,” she says. Pelton says the general consensus is that it takes around three menstrual cycles for hormones to settle again. But for those who have taken the pill for years, it might be longer. “Better skin and mood is associated with longer time on the pill, but the longer women have been on the pill – the more likely they are to report worse skin and mood after they stop using it. So this adds an extra dynamic.” A catch-22.
But even those who have been on the pill a short time aren’t immune from fears about quitting. When Hannah Davis from north London was first put on the combined contraceptive pill at 16 years old, the side effects were instant and drastic. She would wake up, take the pill before school and then, like clockwork, two hours later she would begin feeling nauseous. An hour later, she would be physically sick. She couldn’t keep any food down.
I feel totally hostage to it, I know it isn’t perfect but what if coming off it is worse than being on it?
After three weeks of daily sickness, Davis, now 17, went back to the clinic. After some back and forth – in which she says the doctors reassured her short-term side effects were normal – she was eventually prescribed a progesterone-only mini pill. Although the vomiting stopped, there were other changes on this drug – mood swings, emotions running close to the surface. Now, she would like to quit and stabilise her mood but feels perhaps it is better the devil she knows.
“I feel totally hostage to it, I know it isn’t perfect but what if coming off it is worse than being on it? I go down a rabbit hole of reading the forums and [people’s experiences] are terrifying. I start to think maybe I’ll stay on this forever because I can’t take the risk.” She adds that there is an element of “Stockholm Syndrome” – “I convince myself the pill is perhaps helping me, making things better, and without it I would have worse skin, worse mood swings”.

Joanne*, 21, from Bristol, has been on the combined pill for three years for her acne. But the pill caused fatigue, mood swings and periods of extreme lows she could not control (a study at the University of Copenhagen found women taking either type of pill were more likely to be prescribed antidepressants than those not on contraception). She had wanted to come off the pill for months but felt scared by reading other people's experiences online – of course, this is a self-selecting sample, and as a result likely to be those who have had the worst or best experiences.
But with a void of counternarratives from official sources, it cuts through. “I was terrified of my acne getting worse. Terrified. I felt very much stuck on it”. Amy, 30, from Wolverhampton, who started on the pill at 17, has also been considering quitting for a year but has been deterred by what she reads. “I’d love to be a bit braver with it.”
I felt very much stuck on it
Without more official information, women say they feel uncertain about what awaits them and instead turn to blog posts, forums and outdated magazine articles in a bid to ascertain some roadmap out. Every woman I spoke to was, like me, aware of the unhelpful results that come from a quick Google search on quitting the pill. Molly Rooney, 26, from Merseyside, who has taken the pill for eight years, started considering coming off in Christmas 2019. But like the others, she could only find information in forums filled with other’s experiences of weight gain and adult acne. “I found it really difficult to get a GP appointment to speak about it and I almost feel it’s too trivial to waste their time in a pandemic.”
The Brook sexual health charity is clearer than the NHS on what changes you might expect (acne or skin problems), but crucially says “everyone reacts slightly differently to coming off the pill”. Sarah Mulindwa, a sexual health nurse, explains: “Acne outbreaks are unfortunately to be expected in a high number of women once they stop taking the pill, even if they’ve never had [it] before. The contraceptive pill suppresses your hormones, so when you go off it, your skin will more than likely break out.” She also says it can impact your sex drive. “It is completely normal to feel anxious about stopping the pill, but remember, some women can and do stop contraception with no minimal issues.”
For some, taking the risk has been worth it. Roxanne Cooper-Costello, 22, from Bournemouth, had been on the combined pill since 17 but came off it after it made her “an utter savage to be around” and she felt her pill was in control of her. In the lead up to stopping she watched “tons” of YouTube videos of women documenting their experiences. “I was so uneducated on what was happening to my body,” she says. But the leap of faith paid off. “The first day I had this sigh of relief that I had finally done it and didn’t feel like a slave to it anymore.”
Mulindwa says that women can expect it to take up to three months for the body to return to its normal menstrual cycle, and when this stabilises most will see an improvement in related-issues like acne.
For many women who are prescribed the pill as teenagers it is the inevitable cliff edge we have to face as we enter the next chapter of our lives
Dr Paula Baraitser, of SH:24 sexual health clinic, says for anyone coming off it is about weighing the advantages and disadvantages. “With the combined pill that might be trading the advantages (less acne, lighter periods, controllable bleeding) and the disadvantages (headache, nausea, breast tenderness and possibly mood changes). These are difficult and complicated decisions and the factors [life circumstances, relationships and sexual lifestyles] influencing them change over time.” She encourages women to keep records and revisit decisions regularly.
As we mark the 60-year anniversary of one of the greatest medical innovations for women's rights in recorded history, it is worth considering that we have work yet to do. While the pool of research on side effects is growing (although notably such side effects are still not tolerated in male clinical pill studies) we still have little information about what women should expect when they quit, and how to navigate this time. Instead they are lumped into a homogenous group of women, seen as motivated only by getting pregnant, and concerned with when periods might start up again for this purpose.
It has been 58 days since I last took my pill. After taking it everywhere from school to university, post-graduate studies, 12 homes, two years living abroad, three long-term partners, and everyone in between, it was one of the longest relationships I’ve ever had. After years of deliberation, lockdown gave me the type of clean run I’d never anticipated, hidden away from the world in case the post-pill monsters rear their heads. For many women who are prescribed the pill as teenagers – with few questions asked and little information given – it is the inevitable cliff edge we have to face as we enter the next chapter of our lives.


Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments