‘My son died of sepsis – he would still be here if we had been given a second opinion’
Melissa Mead was told she was ‘worrying too much’ because she was a first time mother

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A mother backing calls for parents to be given second opinions from doctors dealing with their children says the NHS missed 16 chances to save her son from sepsis.
Melissa Mead’s one-year-old boy William died in December 2014, three months after she first raised concerns about his health. She claims she was dismissed by doctors and 111 call handlers when trying to get help for his undiagnosed chest infection that later developed into a fatal condition.
The 36-year-old has now spoken out in support of “Martha’s rule” – a campaign to give families and patients the right to a second assessment if they feel their concerns are not being taken seriously.
Merope Mills created the appeal after her daughter Martha Mills also died from sepsis in October 2021.
Have you had a similar experience? If so email lydia.patrick@independent.co.uk
Ms Mead first noticed her son William was under the weather when he developed a cough but says she was repeatedly dismissed by healthcare professionals who put his symptoms down to a viral infection.
William died 36 hours after his final trip to the GP where Ms Mead says a doctor told her it was “nothing grisly” and that her baby needed rest.
Ms Mead from Penryn, Cornwall, said: “Martha’s story is very similar to William’s, we weren’t listened to, as parents we surely have the right to a second opinion.
“If we had seen just one other person, William could be alive. Plans for his childhood, plans for his future were all stolen from us.
“He was the happiest, loveliest baby, he was so placid and calm – he made being a mum easy, he made my life complete.
“He didn’t get to go to school and I never got to hear mummy I love you. He could have and should have survived.”

Ms Mead, an ambassador for the UK Sepsis Trust, is supporting fellow mother, Ms Mills, who lost her 13 year-old daughter after medical professionals failed to act quickly enough when she contracted sepsis.
The girl sustained a pancreatic injury in a bike accident on holiday with her family and the inquest into her death revealed she would have probably survived if consultants made a decision to move her to intensive care sooner.
Seven years earlier, Ms Mead faced the same inadequacies in the NHS where her son’s case of streptococcus A and pneumonia and later sepsis were misdiagnosed.
Ms Mead first took William to the GP in October 2014 with an “everyday” cough.
She added: “We wanted reassurance, but we were given false reassurance. We were told it was a viral infection. The amount of times I was told ‘you’re a first time mum, you’re bound to be worried’.”
Over the course of the next two months, William’s health deteriorated but she was told there was no cause for concern.
In December 2014, the mother took William to the GP as he became more unwell and started to lose weight.

According to Ms Mead, she was ignored when she argued her son simply “wasn’t right” as her son had lost weight and his temperature was over 40C.
She says the doctor didn’t make a written record of his temperature and didn’t listen to his heart rate or take his capillary or respiratory rate.
The mother and son returned home and William’s condition got significantly worse prompting the mother to call 111 twice.
Both times William’s symptoms weren’t flagged as potentially fatal – Ms Mead followed doctor’s orders and put her boy to bed.
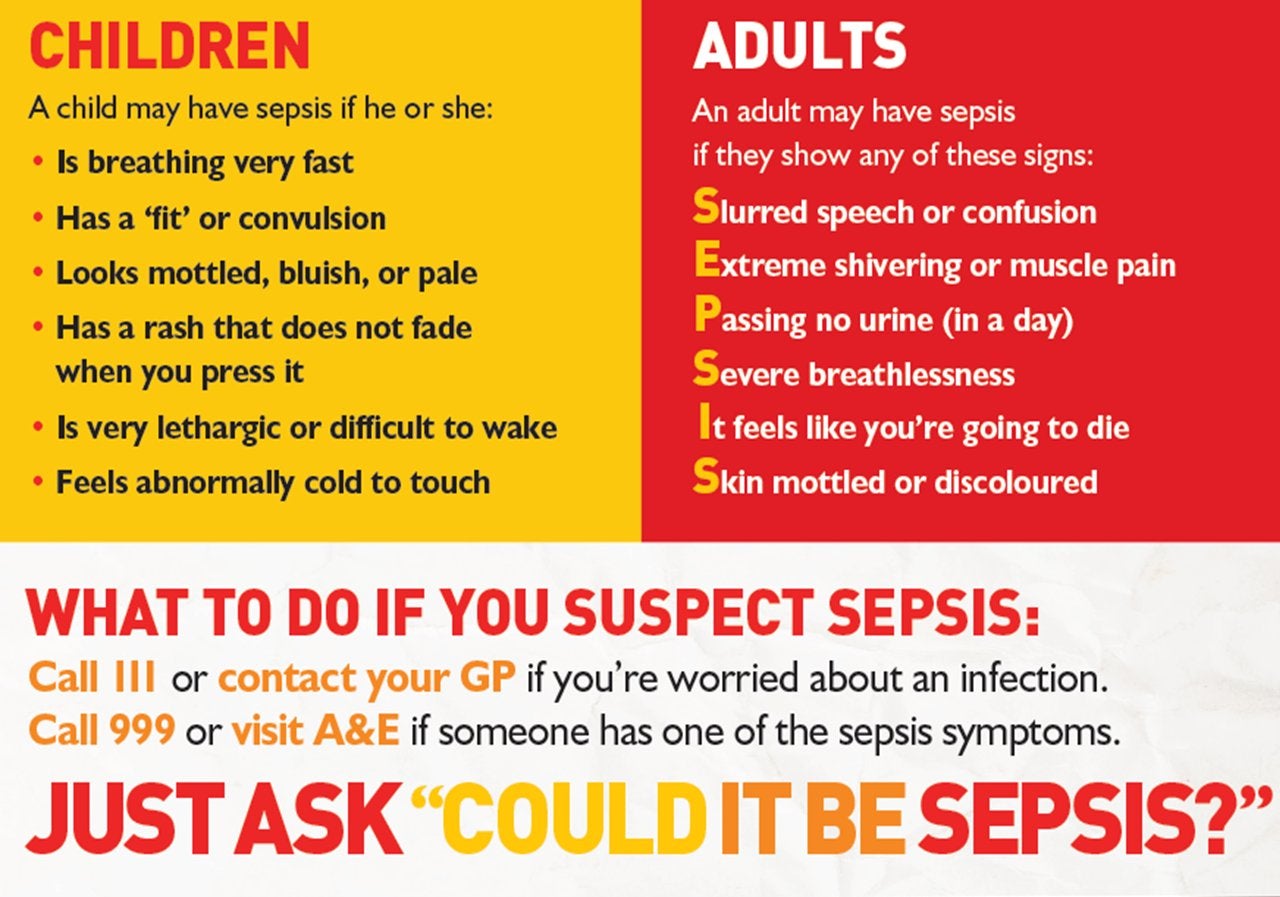
She said: “We were told not to take him to A&E as his condition was non-urgent. Now I know he had every symptom of sepsis such as not wetting his nappy, making a whining, bleating sound and he was cold to touch.
“If I had known the symptoms, I would have been to A&E faster than we can say sepsis.”
The next morning, Ms Mead entered William’s room to find her son lifeless.

She said: “I went over to him, he wasn’t responding, I lightly put my arms through the bar of his cot, it was obvious he was dead. I started the indescribable survival journey of child death.”
Instead of being able to grieve, Ms Mead had to embark on a two year investigation into NHS England.
In January 2016, the NHS England investigation concluded finding 16 failings in care and four missed opportunities to save the one-year-old’s life.
Calling the death a “tragedy”, an NHS England spokesperson said at the time “experts from the UK Sepsis Trust, the Royal College of Paediatrics and Child Health and the NHS are already working to prevent future similar tragic events”.
He added: “We have also recognised the need for GP out-of-hours and 111 services to work seamlessly, and they are now being combined on a rolling basis across England.”
The former secretary of health and social care Jeremy Hunt apologised to Ms Mead for the failings leading to her son’s death in 2014.
Mr Hunt said at the time: “I have met William’s mother, Melissa, who spoke incredibly movingly about the loss of her son. Quite simply, we let her, her family and William down in the worst possible way through serious failings in the NHS care that was offered, and I want to apologise to them, on behalf of the government and the NHS, for what happened.”
Ms Mead says: “I said to Jeremy, the best apology is changed behaviour, but behaviour is still the issue
“There is a hierarchical culture issue of ‘doctor knows best.’ No one knew William better than me and his dad like no one knows Martha better than her mum and dad.”



Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments