My poor old creaky bones: Meet the millennial women with arthritis
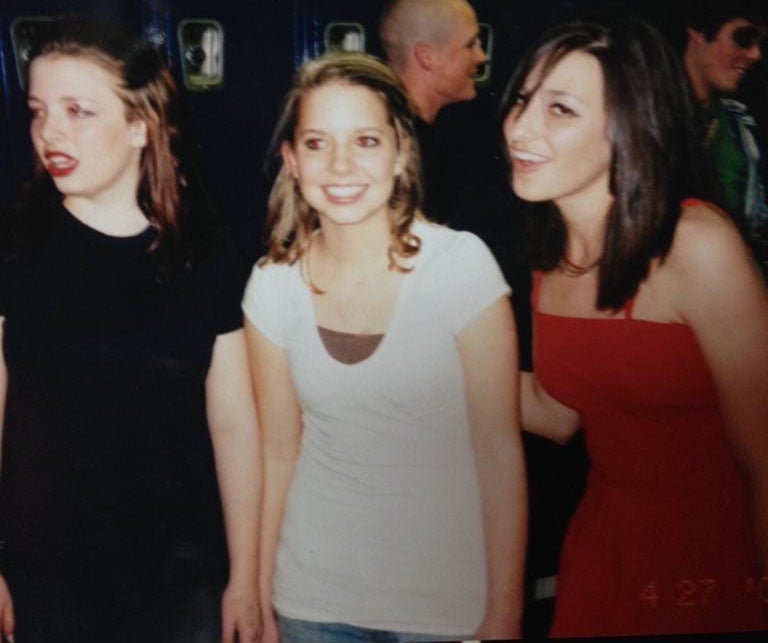
Although it's commonly thought of as an old person's disease, arthritis affects 27,000 people under the age of 25 in Britain, including Olivia Campbell


My name is Olivia and I have rheumatoid arthritis. As I write this article my fingers and wrists scream in pain while I repeat the same keyboard motion over and over. They will hurt like hell later. I was 14 when I realised something wasn’t right with my body. It was the beginning of 2011, and the aching in my foot that had started months before was getting worse and worse until I could ignore it no longer.
My middle finger on my right hand was normal, until one day it wasn’t. This was when the comments started. Offhand remarks from my mum saying I walked like an old woman, while people started casually asking me if there was something wrong with my legs. “No,” I’d tell them, unsure myself what was happening.
When you hear the word arthritis you’d be forgiven for thinking that it is something that only effects our elderly population. A word that evokes images of stiff joints and creacking bones and stereotypes that are given to people who’ve reached a ripe old age, not women in the prime of their lives.
The reality, however, couldn’t be more different. Arthritis is a disease that doesn’t discriminate against any age. There are babies who are born with it, teenagers who develop it and a whole host of other groups who are a just as likely to experience some form of arthritis.
I was diagnosed when I was 15 and since then the disease has always been at the periphery of my mind. At that age, my thoughts were preoccupied with the fact that my auntie was getting married in two weeks and I was to be her bridesmaid, not the fact that my bones were beginning a journey that will eventually end with them being eroded away. Arthritis has the potential to dominate my entire life and I know that I am not alone.
Arthritis Research UK estimates that nearly 10 million people in the UK suffer from some form of the condition, with the most common strand, rheumatoid arthritis (RA), affecting more than 400,000 adults. This means that more than 1 per cent of the adult population has the disease. It is also believed that as many as 27,000 people under 25 are living with the condition in some form.
In a cruel twist of fate, women are three times more likely to develop arthritis than men. For women, the disease comes with its own set of problems that are unlikely to be experienced by male sufferers. Pregnancy, messed-up hormones or the simple act of not being able to wear fancy shoes are just some of the things that female sufferers have to contend with.
But what exactly is arthritis? This a complicated question as there are actually more than 200 types which can affect the body in different ways. In a nutshell, arthritis is a name given to a group of conditions that cause joint pain and inflammation. RA is an autoimmune disease where the body’s immune system targets the areas around the joints, causing inflammation, swelling joints and varying levels of pain. Over time, the joints and bones will begin to wear away.
* * *
Nicolle Okoren was 14 when she was diagnosed with rheumatoid arthritis. “The pain started in my wrist,” she says, massaging her joints while she does so. “I was taking piano and violin lessons so doctors initially thought it was carpal tunnel syndrome from playing so much. But then my ankles and feet started killing. Soon it was my knees and my elbows. It spread so quickly. I remember spending most of that summer in bed, unable to move because everything hurt so badly. I was actually walking on the sides of my feet because putting pressure on my ankles hurt so much.”
I got it really badly in my jaw – and I sang a lot too. I don’t do it anymore because of the damage arthritis has done to my voice. I ended up pushing it and developed vocal nodes. I had so much scarring on my throat that I couldn’t speak for a month
Okoren has arthritis in the majority of her joints, including her jaw: “I got it really badly there – and I sang a lot too, it was like my big thing. I don’t do it anymore because of the damage arthritis has done to my voice. Because I couldn’t open my jaw, I ended up pushing it and developed vocal nodes. I actually had so much scarring on my throat that I couldn’t speak for a month.”

Lauren Anderson was also diagnosed with arthritis when she was 22 years old – and has been living with it for five and half years. “It started off as just simple aches and pains and then developed into the disease,” Anderson says. “Until I got the disease myself, I didn’t really think I could get such a condition. It was a bit of a shock, although deep down I think I already knew. I feel like a 20-year-old in an 80-year-old’s body,” she says when asked how she deals with her diagnosis at such a young age
Hannah Dehawnt used to be an artist before she developed the disease at 22. “I’ve lost a lot of the finer movements in my hands. I used to create set designs, building and painting scenery basically, as well lots of illustration and drawing. My disease has changed everything.”
Unlike the other people I interviewed, Dehawnt has only been diagnosed for a year and is only just beginning get used to the tumultuous change that a chronic illness can bring. “There was nothing that was stopping me before – I just got on with my life. Now it’s hard to not feel trapped by my condition. It’s also really daunting because I’m only in my early twenties and this degenerative thing is just going to carry on.”
For people with arthritis, simple things that everyone takes for granted can become almost impossible. You never realise how hard it is to put on tights when your knees are too swollen to bend the right way. Or how hard it is to chop vegetables when your wrists don’t function properly. The collection of movements that make up our everyday lives suddenly become problematic.
The lives of those living with the condition are also defined by flare-ups. It is incredibly hard to predict when one might hit, and if it does, how severe it is going to be. Many women feel like they are living at the mercy of their disease, especially when even something as simple as dressing feels like a mammoth task.
“Pretty much all of my clothes are easy to pull on and off,” Okoren says, gesturing to a grey cardigan she’s wearing. “Butt I’ve told my flatmates that there will days when they’re going to need to help me with getting undressed.”
When Anderson had one of her worst-ever flare-ups five months ago she struggled with everything: “I couldn’t wash myself – I couldn’t get in and out of the bath. I struggled to dress myself. Even going out for a walk to try and clear my head was near-impossible.”
Hair also plays a key role in many women’s identities, so imagine how hard it can be when your body won’t even allow you to create a pony-tail. “All my closest friends in college know that my hair was in a messy bun I’ve had a really bad flare-up that day,” Okoren says. “It’s a frustrating feeling when I can’t even lift my hands up and make something as simple as my hairstyle happen.”
It’s hard to feel betrayed by your own body when your hands won’t even let you do something as simple as opening a carton of apple juice. Medication is also a source of contention for those with the condition. Methotrexate is a drug that sufferers will have a love or hate relationship with. It’s a problematic one.
Although it is the most effective and widely used medication that helps deal with the symptoms of the disease, the immunosuppressant drug comes with a myriad of unpleasant – and sometimes life-altering – side effects, including nausea, fatigue and vomiting. Hair follicles are also affected which can lead to hair loss.
More severe side effects include liver disease, lung disease and lymphoma – although these are rare. Methotrexate is actually a chemotherapy drug which is often used (in much higher doses) to treat cancer. The treatment works by reducing the activity of the immune system, thus reducing attacks on the joints. However, the drug does leave the body more prone to infection.
I was extremely lucky in that the only negative experience I had with the drug was when I forgot to take my folic acid and it felt like someone was plunging a tiny sword right into my liver.
However, a lot of people aren’t so fortunate. A study in 2009 found that 73 per cent of all rheumatoid patients have at least one side effect associated with a drug. Furthermore, at least 16 per cent of patients have been forced to stop using it altogether. “When I was on Methotrexate it completely messed up my gut,” Okoren says. “I have to be extremely cautious of what I eat now because my medication has caused my stomach to become to so ulcer-ridden.”
She was only on the drug for a couple of months but she’s still feeling its effects even now.
Anderson also suffered when she was on it: “It was dreadful. I ended up getting mouth ulcers and extremely severe stomach pain every time I took it. When it’s a weekly thing it becomes unbearable. When you’re feeling nauseous five out of seven days you begin to ask yourself whether not feeling joint pain is even worth it.” Taking Methotrexate is not a light decision and one that for many sufferers will mean weighing up the risks.
Dehawnt didn’t even get to that stage. She failed the lung tests required and her results showed her immune system would not be strong enough to deal with any sort of attack. Instead she was put on sulfasalazine, a drug which appeared to give her a lifeline. For the first time in at least two years Dehawnt felt some reprieve from the chronic pain in her joints.

However, this relief turned out to be fleeting. A routine blood test revealed that her blood cell count had dropped dangerously low and she was taken of it. “I sat there and cried,” she says. “I’d been given an injection of life and now it was being taken away from me.”
Dehawnt currently isn’t on any medication and is living on pain killers and antioxidants while doctors try and figure out another path. This is the reality for many sufferers.
* * *
Like many conditions, not just autoimmune diseases, pregnancy can be a serious source of contention for sufferers. But what is the reality for women who want to embark on the road to motherhood? Joanne Sample discovered she had arthritis when she was pregnant with her second child, Billy. “One day I just couldn’t move my arms properly and my joints were really inflamed. I was diagnosed within 24 hours of the flare-up and since then, my arthritis hasn’t really gone into remission.”
There is a known phenomenon among arthritic women who are pregnant: symptoms can often disappear for the entirety of the pregnancy. It is believed that the influx of hormones in the body have a positive effect – something which Sample experienced herself in her following two pregnancies. The real problem, Sample says, came after the birth of her son. “About three weeks after Billy’s birth, the pain hit me like a ton of bricks,” she says. “This was the moment I realised how severe it was.”
About three weeks after Billy’s birth, the pain hit me like a ton of bricks. This was the moment I realised how severe it was
Those who’ve been in remission often find their arthritis will return up to six to 12 weeks after delivery. Post-pregnancy is tough for any women, but for women with the condition it is undoubtedly more difficult. Simple things like carrying the baby or being able to change a nappy can become incredibly complex when your hands refuse to cooperate. Sample laments the excessive use of buttons and poppers on children’s clothing, something she laughs about but still struggles with it.
However, the problems can start even before a woman gets pregnant. Methotrexate, which Sample and many other women are on, can be particularly problematic for women carrying children. The widely used drug is actually an abortifacient and is commonly used to terminate pregnancy in the early stages. The medication has also been linked to birth defects including congenital heart defects.
Sample was still on Methotrexate when she unexpectedly became pregnant with her fourth child, Ava. “After the birth of my third child I was told I probably wouldn’t be able to have any more children,” she says. “When we found out about Ava, we were really worried about the drugs I was still on and the effect it could have on her.”

Her pregnancy was a whirl of hospital appointments to constantly monitor the life developing inside of her. Sample was told that it was highly likely her child would not survive and if she did, could face serious medical problems from birth. “When Ava was born, we quickly realised that the medication had caused some damage,” she says. “She can’t digest protein and as a result she has a few feeding problems. She is also constantly being monitored for heart and nerve problems in case something hasn’t been diagnosed yet.”
However, despite all this, Ava “is really turning a corner. She really is my little miracle”.
It’s inevitable that when a disease can be so destructive on the body what little discourse there is focuses on the physical toll it can take. However, Anderson says, not enough focus is being placed on mental health. “The biggest struggle for me is not the physical element but the mental,” she says. “No one can understand unless you’ve got it. The disease takes away small things in your life but then they all add up. I really don’t think there is enough support for mental health.”
She argues that the state should be giving the option for sufferers to receive therapy or counselling on the NHS as a way of alleviating the emotional toll the disease can have. Arthritis is an extremely misunderstood disease in all parts of society. “It can feel like a very lonely disease,” Anderson says.
“People often don’t see the disease and don’t really believe you,” claims Okoren. “I would push myself way further because I felt I had to adjust to other people’s view of ‘normal’. It’s created a complex where I often don’t trust my feelings.”
People often don’t see the disease and don’t really believe you. I would push myself way further because I felt I had to adjust to other people’s view of ‘normal’
A 2018 study published by charity, Versus Arthritis, estimates that at least 73 per cent of all 16-34 years old with the condition feel loneliness of a regular basis. Furthermore, at least 54 per cent of young people have experienced mental health problems including depression or anxiety since being diagnosed.
Andrea McBride, a rheumatology nurse specialist and founder of Arthur’s Place, a social networking site for young people with the disease, agrees: “I have 12 years’ experience in rheumatology and one of the hardest things to see is how lonely and isolating these conditions can be, especially among young adults. Whether it’s down to a lack of representation in the media or lack of understanding about arthritis, the impact is that far too many young people affected feel like they can’t reach out.”
Indeed, society’s penchant for dismissing invisible illnesses has a detrimental impact on any person, not just those with the disease.
Before I was given my diagnosis of rheumatoid arthritis, I went undiagnosed for four years. The swelling in my knee that prevented me from walking at least twice was put down to randomness by my GP. The constant pain in my ankles and fingers were “growing pains”.
When seeking out other women for this article I came across countless other stories of women who’d gone undiagnosed by their GPs or doctors despite showing symptoms. Others spoke of being given completely different diagnosis’ altogether. One woman told me that by the time she’d been given the correct diagnosis, the damage that had been done to her joints so far was irreparable.
“I don’t think GPs are very clued up on it,” Anderson says. “Health professional or not, people still aren’t aware enough of how rife it is in young people. My GP wasn’t interested. I think the age factor is still the biggest issue even among health-care professionals.”
I spoke to McBride about her insights about diagnosis. “When we have an injury, diagnosis and treatment can be black and white,” she says. “When it comes to inflammatory conditions, diagnosis is a bit like collecting pieces of a jigsaw that are gathered over time. Things such as family history to investigations like blood tests, and sometimes response to treatments, all come together to form the most comprehensive picture possible, so a diagnosis can be confirmed.”
When it comes to inflammatory conditions, diagnosis is a bit like collecting pieces of a jigsaw that are gathered over time
When a condition can be so life-changing it is easy to get lost in something that can be construed as a “doom and gloom” attitude. However, there are thousands of people, not just young women, who are thriving with the disease and refusing to let it beat them. Life doesn’t have to grind to a halt when a diagnosis is given.
Dehawnt is beginning to paint again. She’s finding new ways to be creative, something which she thought her arthritis had taken away forever. Anderson says she will continue to laugh at her condition at times when she feels like crying. And she will continue educating people about the complexities of arthritis.
“I’ve really learnt how strong and independent I am because of my condition,” Okoren says. “I know what it feels like to hurt so badly or to feel so alone in it and not see an end in sight. I have a lot of compassion for anyone who feels pain. I think that it is a really beautiful thing.”
“I’m grateful for my arthritis. I’m not happy that I have it, but I am grateful.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments