Pandemics will prosper unless people with HIV are put first
Treating HIV as a priority will not only save lives from coronavirus but also reduce the risk of new variants spreading worldwide, writes Kieran Guilbert on World Aids Day

While all eyes are on the omicron Covid-19 variant that has triggered global alarm, Wednesday marks the annual commemoration of another deadly disease that has claimed millions of lives.
Established in 1988, World Aids Day asks us to remember those who have died from HIV-related causes, to provide support for those living with the virus, and analyse progress towards a target of ending Aids by 2030.
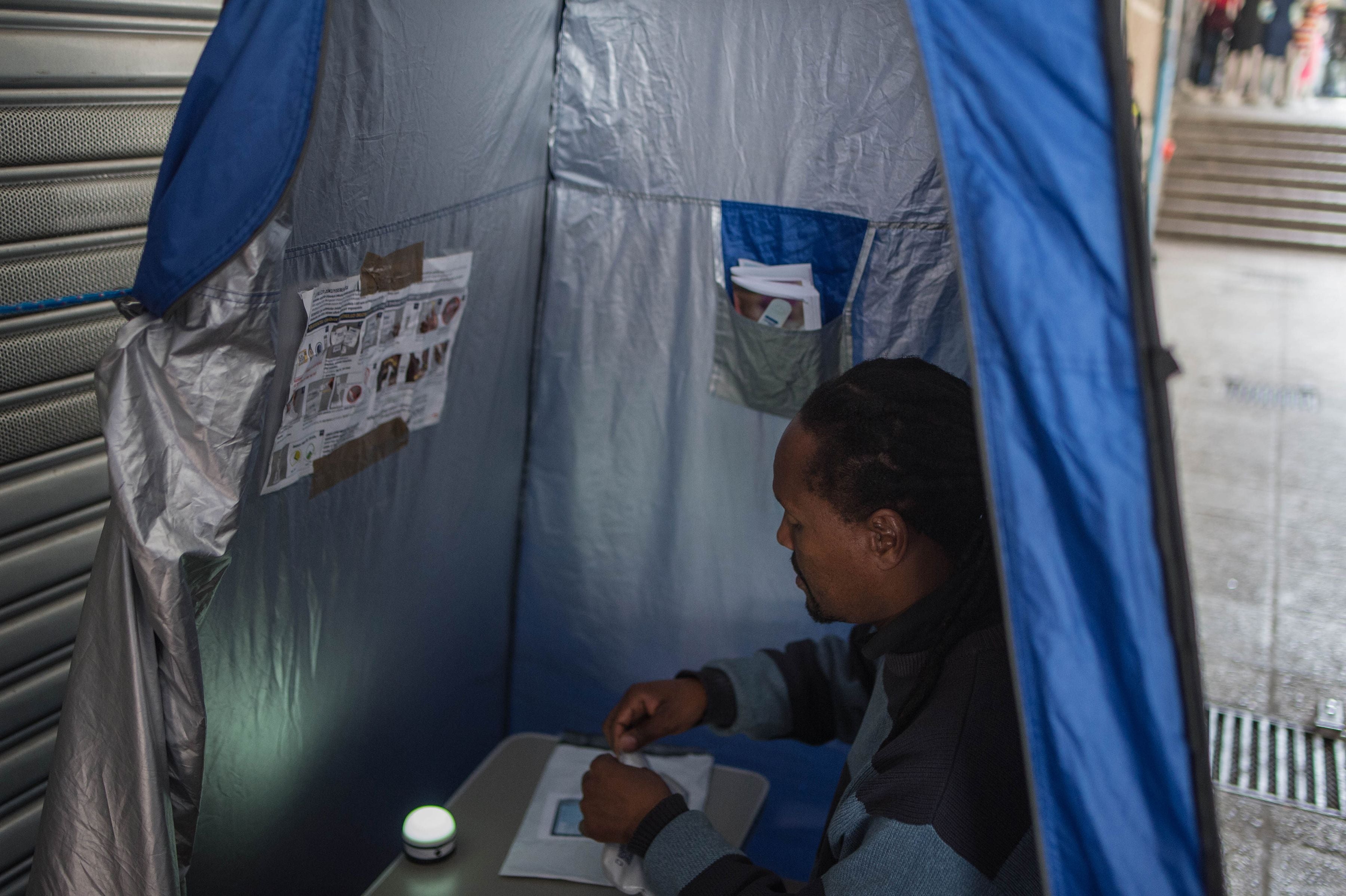
But this year is different. The fight against HIV has taken on new significance since the coronavirus pandemic upended life as we know it, nowhere more so than in sub-Saharan Africa. It is home to more than two-thirds of the almost 38 million people estimated to be living with HIV, but less than 5 per cent of its 1.14 billion population has been fully vaccinated against Covid-19.
Health systems across the continent have been stretched to breaking point by the pandemic, scant resources have been diverted towards coronavirus at the expense of tackling other diseases, while measures such as lockdowns have hindered HIV prevention and treatment efforts.
To compound matters, a WHO report in July found that people with HIV are 30 per cent more likely to fall critically ill or die from Covid-19, while scientists tracking the omicron coronavirus variant believe it may have evolved in an immuno-compromised person, possibly with untreated HIV.
What does this mean? Not only are people with HIV far more vulnerable to coronavirus, those who do not know they have the disease or lack treatment could act as the source of future mutations.
Focusing on South Africa puts the problem into stark perspective. Less than a quarter of its 60 million population are fully vaccinated against Covid-19. At least 8.2 million South Africans are infected with HIV, but only about 71 per cent are being treated with life-saving antiretroviral drugs.
To keep up to speed with all the latest opinions and comment sign up to our free weekly Voices newsletter by clicking here
The solution is simple: prioritise people with HIV for Covid-19 vaccines. Yet an informal WHO poll earlier this year of 100 countries found that only 40 had done just that. Moreover, as a recent editorial in The Lancet medical journal argued, treating HIV will not just save lives now but help protect the global population from future pandemics.
But worryingly, targets for tackling HIV are not being met. Last year there were 1.5 million new infections and about 690,000 Aids-related deaths – far above the 500,000 goal for each metric.
The head of UNAIDS, Winnie Byanyima, put it bluntly, in terms that should trouble us all. “We cannot be forced to choose between ending the Aids pandemic today and preparing for the pandemics of tomorrow,” she said. “The only successful approach will achieve both. As of now, we are not on track to achieve either.”
Yours,
Kieran Guilbert
Deputy international editor






Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments