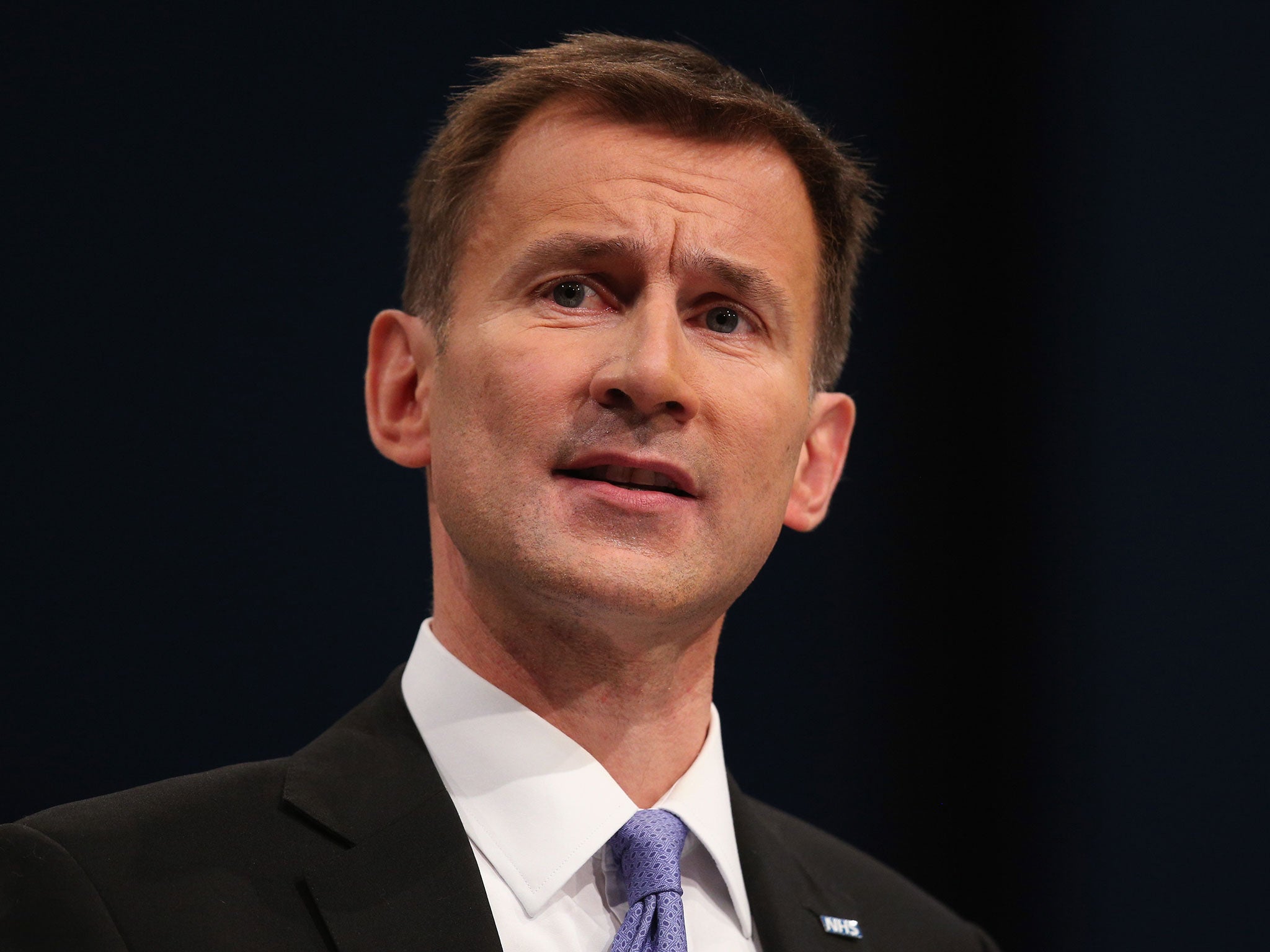
Jeremy Hunt 'misrepresenting' data on weekend death rates at NHS hospitals, says research surgeon
Dr Peter Holt said his research was wrongly being used to support the Government's push to change junior doctors' contracts
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A doctor who was part of a study on links between staffing and deaths in the NHS has accused the Government of “continually misrepresenting” the findings to support its push to change junior contracts.
Dr Peter Holt, a vascular surgeon at St George's University of London, said he had written to Jeremy Hunt, the Health Select Committee and shadow Health Secretary Heidi Alexander raising his objection.
In a post on the Junior Doctors contract forum Facebook group, he wrote that the research published in December “could never have shown that higher staffing on weekends reduced mortality”.
“We did not have staffing levels by day of the week but aggregated data over a time period, so we didn’t even investigate this,” he added.
“The data have been continually misrepresented. I have put this in writing to the Secretary of State, Heidi Alexander and Health Select Committee.
“I have asked the latter for a minuted retraction of the way in which the evidence is being used and acknowledgement of this. No replies so far.”
The paper, published in the British Journal of Anaesthesia, analysed data involving nearly 295,000 patients to find that fewer patients die after emergency surgery in hospitals that have more doctors and nurses.
It indicated a direct link between the numbers of doctors, nurses and senior clinicians working in a hospital and the patient’s chances of survival.

Researchers found that the likelihood of death was 11 per cent higher where the patients was admitted to hospital at the weekend while the likelihood of death was seven per cent higher in trusts with the lowest numbers of nurses per bed.
In a press release marking the publication, Dr Holt was quoted as saying: “This is the first analysis on this scale for emergency general surgical admissions examining the associations between the numbers of senior doctors, junior doctors and nurses per hospital bed and patient survival rates.
“Although we have not demonstrated causation, we believe the findings should form an important part of the debate over disparities in staffing levels and resource provision between NHS Trusts.”
The study could be one of eight cited by Mr Hunt as evidence of higher weekend mortality rate, as he announced plans to enforce controversial changes to junior doctors’ contracts in the House of Commons on Thursday.
“Six of those say staffing levels are a factor that needs to be investigated,“ he added.
”Professor Sir Bruce Keogh describes the status quo as ‘an avoidable weekend effect which if addressed could save lives’ and has set out the 10 clinical standards necessary to remedy this.

“Today we are taking one important step necessary to make this possible.”
The new terms, which will come into force for junior doctors in England this August, classify Saturday as a normal working day and extend “social” hours to cut those awarded extra pay.
They have been the subject of two strikes by junior doctors with the British Medical Association union so far and have seen huge opposition from NHS employees.
Concern has been raised over the Government’s use of several scientific studies to support its move towards a “seven-day NHS”.
Fiona Godlee, editor of the British Medical Journal, wrote to Mr Hunt with concerns he had “misrepresented” another study on weekend mortality and inferred that the deaths were avoidable, when the research did not make that clear.
Research carried out by two paediatricians last year also alleged that the Health Secretary’s comments claiming that people were more likely to die if they attend hospital at weekends were also responsible for mortality rates.
In a letter to the BMJ, they identified a “Hunt effect” causing people to delay seeking treatment until a weekday despite being ill because of concerns sparked by the Conservative MP’s statements.
Two deaths were reported as a result of the delay and a third of people suffered “long-term, irreversible morbidity” in surveyed cases involving intensive care, surgery, psychiatry, medicine, child health and obstetrics and gynaecology.
The Department of Health has not yet replied to the Independent’s request for a comment on Dr Holt’s complaint.
“There is clear independent clinical evidence that standards of care are not uniform across the week and this Government makes no apology for tackling the problem to make sure all patients receive the same high quality care seven days a week,” a spokesperson previously said.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments