Pioneering global study to explore why Black people suffer more aggressive cancers
Researchers from across the UK, USA, and Africa have been awarded £21m to examine the causes of higher death rates for Black patients
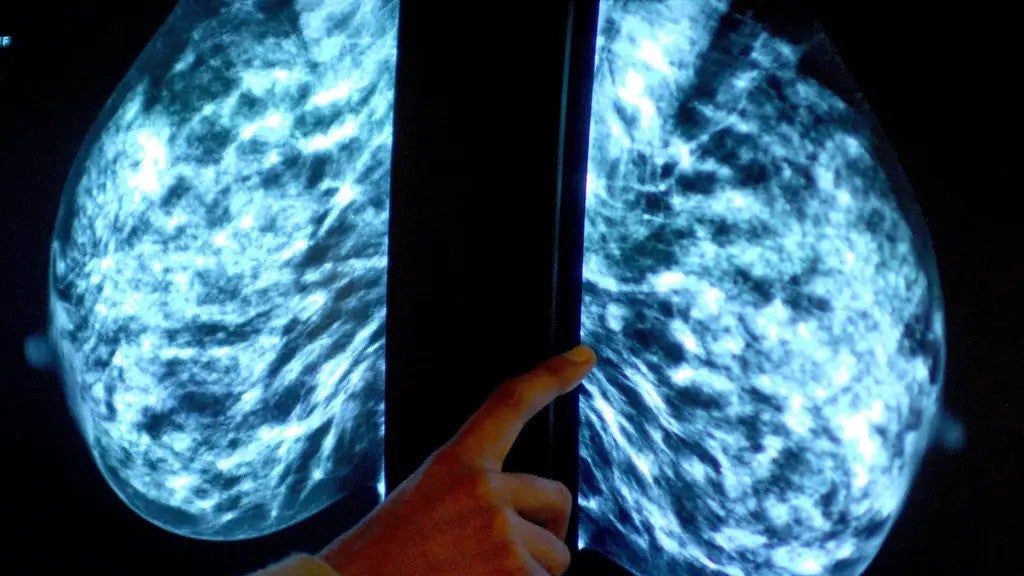
A five-year, multimillion-pound investigation has been launched into why Black people are more likely to develop more aggressive forms of prostate, breast and pancreatic cancers.
These illnesses disproportionately affect people within ethnic minority groups, with higher mortality rates and earlier onset of the disease, compared to their white counterparts.
Researchers from across the UK, USA, and Africa have been awarded £21m to examine the causes of these inequalities among Black people, through the Cancer Grand Challenges funding from Cancer Research UK and the US National Cancer Institute.
The study will be co-led by Isidro Cortes-Ciriano, from the European Bioinformatics Institute in Cambridge, who described this project as an “exciting” and “major step forward for understanding and tackling cancer inequities”.
“This is crucial for dissecting the complex interplay of social, genetic and environmental factors contributing to cancer,” said Dr Cortes-Ciriano.
“This project will advance our understanding of cancer in people of African descent and help to make a difference in the lives of those disproportionately affected by this disease.”
Black women in England are up to two times more likely than white British women to receive a late-stage diagnosis for breast, ovarian, uterine, non-small cell lung cancer and colon cancer, a landmark study published last January revealed.
When it comes to cancer, early detection is crucial: late diagnoses mean that the disease is generally harder to treat.
In August, Dr Habib Naqvi, chief executive of the NHS Race and Health Observatory, warned that there is a “broad misperception” that Black women “don’t suffer as much from breast cancer”, which can result in the perception that “cancer is a white person’s disease”.
Equally alarming, Black men face twice the risk of dying from prostate cancer compared to white men.
“We know the number of cancer cases diagnosed in ethnic minority groups is likely to grow over time, meaning that without any action, this gap will continue to widen,” Cancer Research UK chief executive Michelle Mitchell said at the time.
The reasons for these disparities vary and contributing factors include a lack of awareness, distrust in healthcare systems, delays in seeking help and barriers to accessing diagnostic tests.
Stigma and myths around cancer in Black communities can also play a part.
Healthcare professionals and campaigners have called for urgent, targeted research and strategies to address these inequities.
The newly-assembled team of experts will be working under “Project SAMBAI” – Societal, Ancestry, Molecular and Biological Analyses of Inequalities – and analysing social, environmental, genetic and immunological factors around the diseases.
They aim to create a global resource that can be used to define the factors that cause and influence disparate outcomes in diverse, underserved populations.
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies