Doctor 'called off' attempts to save six-year-old boy after mistaking him for another patient
Court hears that death of Jake Adcock, who had Down's Syndrome, was down to 'serious neglect' of hospital staff
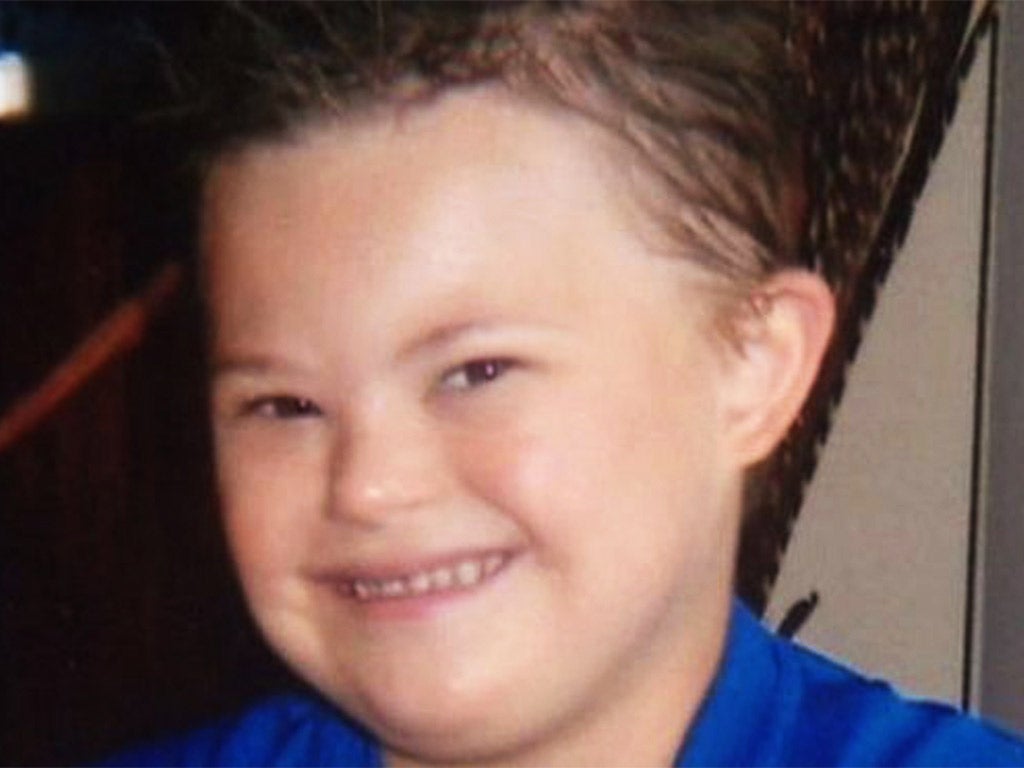
A six-year-old boy died because of “serious neglect” by hospital staff, including a doctor who called off attempts to save him because she had mistaken him for another patient, a court has heard.
Jack Adcock, who had Down’s Syndrome, died at Leicester Royal Infirmary in February 2011 after being admitted while suffering from vomiting and diarrhoea. He developed pneumonia and septic shock and died later that day. Dr Hadiza Bawa-Garba, who denies manslaughter due to negligence, believed the boy had been placed under a “do not resuscitate” order, a trial at Nottingham Crown Court heard.
As a result of this “remarkable error”, medical staff were stopped from giving life-saving treatment to the youngster by the doctor, prosecutor Andrew Thomas QC, told the court.

“When she [Dr Bawa-Garba] came into the bay, almost immediately she called the resuscitation off,” he said. “She told the other doctors Jack had been marked down as ‘do not resuscitate’ earlier in the day.”
It was only when the most junior doctor present picked up the boy’s notes and could not find a ‘do not resuscitate’ entry “that Dr Bawa-Garba realised she had got him mixed up with another patient,” he added. This was “powerful evidence of Dr Bawa-Garba’s performance that day,” he said.
He added that while Jack, of Glen Parva, Leicester, was “beyond the point of no return” and that resuscitation was “futile”, it suggested that Dr Bawa-Garba had not given the boy “sufficient care”.
Two other hospital staff, Sister Theresa Taylor, 55, and 47-year-old Portuguese-born agency nurse Isabel Amaro also deny charges of manslaughter through gross negligence.
“We say that Jack’s death was caused wholly or in part by serious neglect on the part of the team on the Children’s Assessment Unit,” Mr Thomas told the jury.
The court heard that Jack had fallen ill during the night and had been admitted to hospital on the advice of his GP. However, medical staff “failed to act on obvious symptoms of serious illness”, he said.
Nurses Amaro and Taylor gave Jack a paediatric observation priority score of four when he was admitted, said the prosecutor, who suggested that a score of seven or eight would have been more accurate. This would have implied that Jack was in a critical condition.

“We say that the failings of each of the defendants contributed significantly to Jack’s death,” he said. “There was of course an underlying natural illness, the lung infection, which had led to sepsis and septic shock. But the lack of care contributed to Jack’s death. It was a needless death.”
Sepsis, a common but potentially life-threatening condition, involves widespread inflammation throughout the body, caused by infection. The medics failed to recognise that the boy’s body was “shutting down” due to sepsis and close to death, said Mr Thomas. He said the staff did not monitor Jack’s condition effectively, and failed to recognise high levels of blood gas and lactate.
The Crown Prosecution Service brought the charges last year following a police investigation into Jack’s death, details of which emerged at a 2013 inquest.
The inquest heard that Jack’s father, Vic Grey, had left the hospital at about 7.20pm when they believed their son was getting better. However, he fell unconscious just an hour later and never recovered.
In a tribute to him, Mr Grey said: “Jack loved life and life loved Jack. The room lit up when he walked in.”
The trial continues and is expected to last up to five weeks.
