The Independent's journalism is supported by our readers. When you purchase through links on our site, we may earn commission.
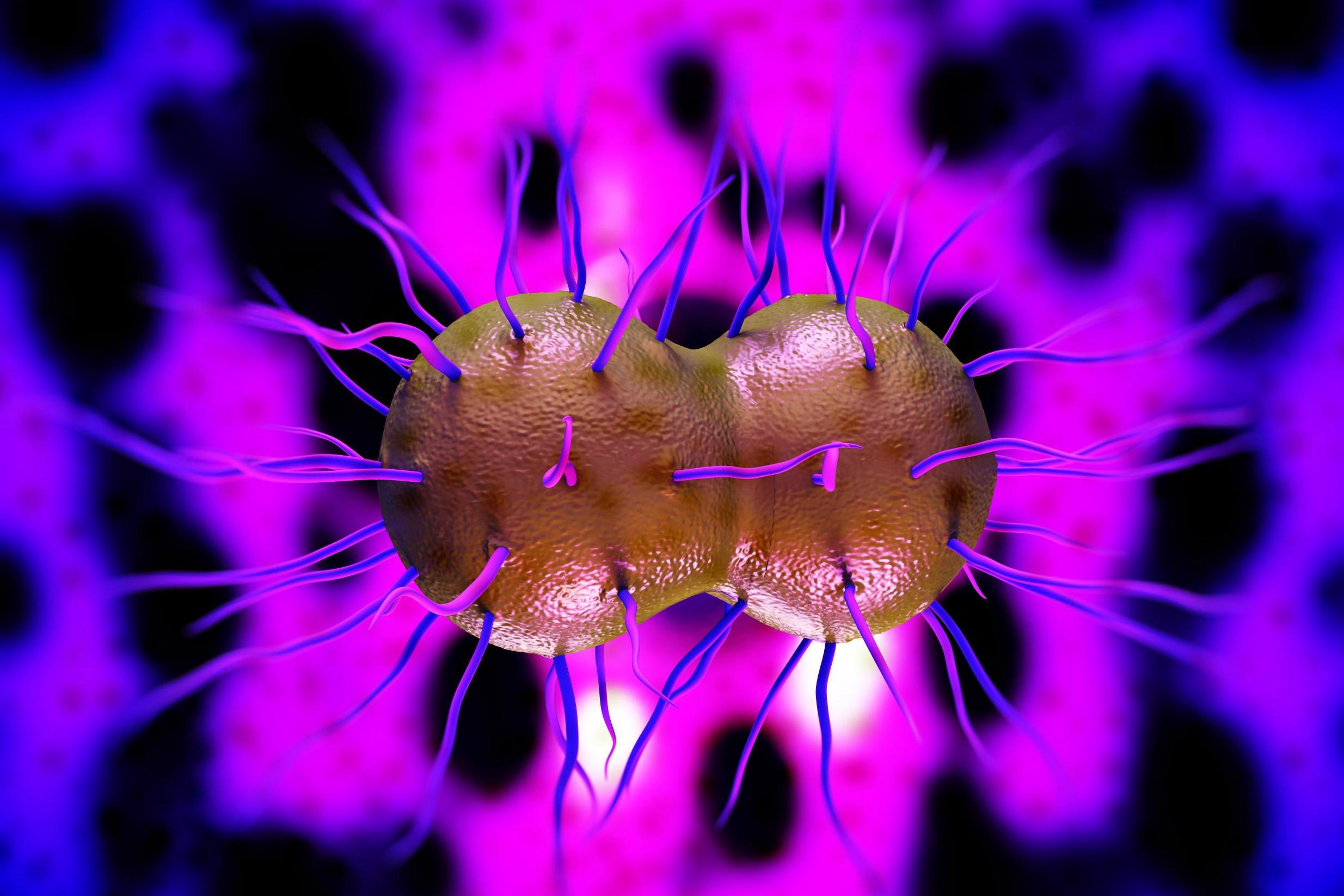
Oral sex is making gonorrhoea harder to treat, warns WHO
‘The throat infections act as a silent reservoir’
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Gonorrhoea is on the rise due to a decline in condom use during oral sex, the World Health Organisation warns.
The drug-resistant STI can spread from the throat of an infected person without them even knowing that they have the disease as in most cases, there are no symptoms.
Subsequently, resistance to treatment via antibiotics is increasing, with more than 50 countries reporting futile use of ESCs – the single medically-approved group of drugs that remain effective in treating the illness.
It's a hugely difficult condition to treat in any case, because there are fewer blood vessels in the throat and therefore it is that much tougher for any antidote to reach the bloodstream.
"Transmission is very efficient from someone who has gonorrhea in their throat to their partner via oral sex," Emilie Alirol from the Global Antibiotics Research and Development Partnership, told The New York Times.
“To control gonorrhoea, we need new tools and systems for better prevention, treatment, earlier diagnosis, and more complete tracking and reporting of new infections, antibiotic use, resistance and treatment failures,” said Dr Marc Sprenger, Director of Antimicrobial Resistance at WHO.
“Specifically, we need new antibiotics, as well as rapid, accurate, point-of-care diagnostic tests – ideally, ones that can predict which antibiotics will work on that particular infection – and longer term, a vaccine to prevent gonorrhoea.”
The latest scare which has supercharged concerns regarding the disease is known as “super gonorrhoea”, which has so far proved impermeable to every treatment on the market.
So far there have been no reported cases of the impervious condition in Britain, but patients have been diagnosed in Japan, France and Spain.
When left untreated, gonorrhoea can lead to a number of severe medical issues that directly affect women, including pelvic inflammatory disease, ectopic pregnancy and infertility, in addition to an increased risk of HIV, the WHO states.
Gonorrhoea is the second most common bacterial STI in the UK, with 35,000 cases reported in England in 2014. Globally, it affects 78 million people per annum.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments