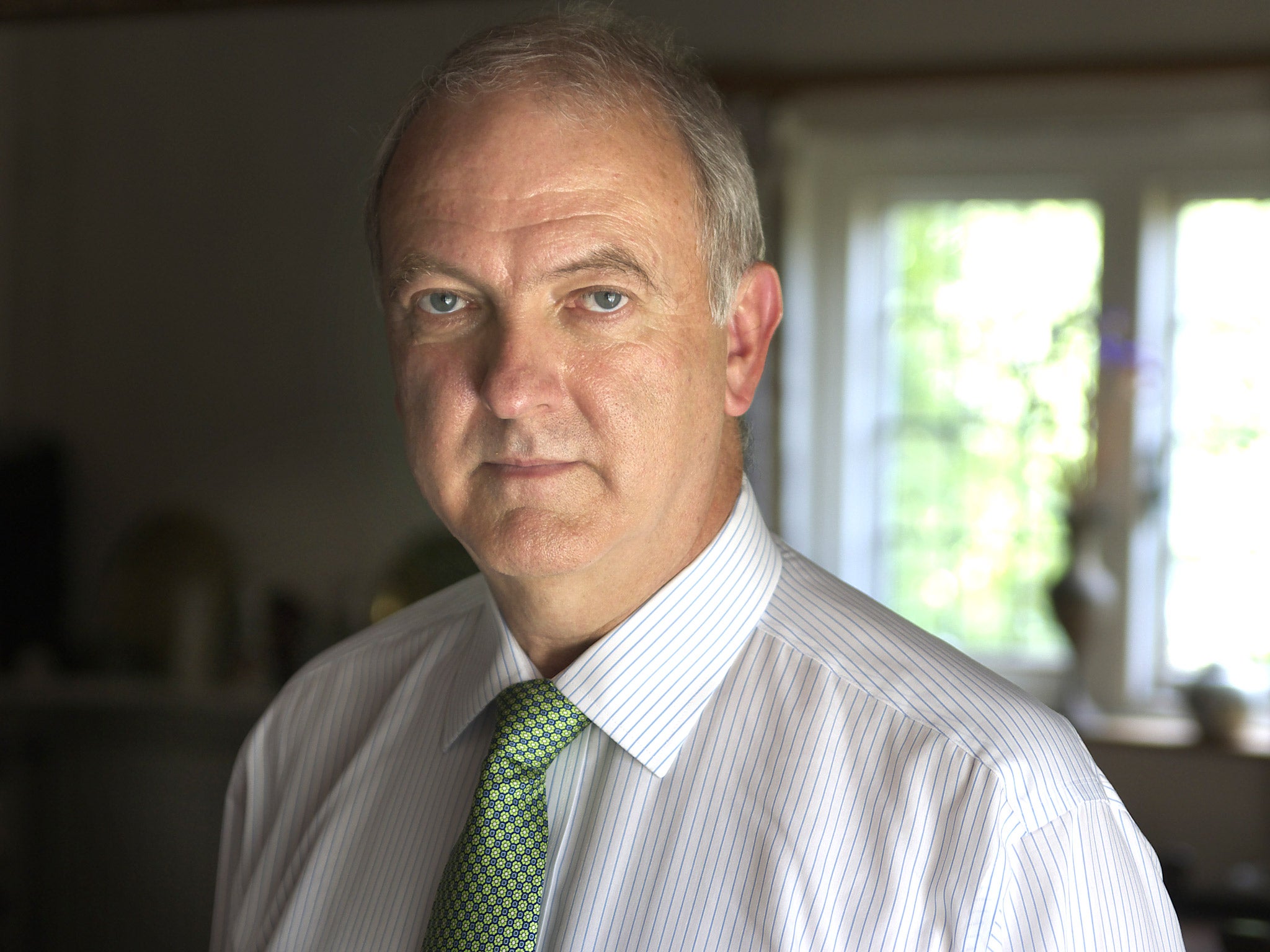
Top doctor calls for two-tier A&E to relieve NHS casualty wards 'creaking at the seams'
Sir Bruce Keogh proposes that GPs, local pharmacists, paramedics and the NHS 111 telephone service should all do more to keep people out of hospital
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.The NHS should have a two-tier A&E system and the role of telephone consultations with GPs and nurses should be greatly expanded to take the pressure off casualty wards that are “creaking at the seams,” England’s top doctor has said, in the biggest proposed shake-up of NHS emergency care since the 1970s.
Sir Bruce Keogh, NHS England’s medical director, said in a report that the majority of patients with minor conditions should be treated “as close to home as possible”, while treatment for the most serious medical emergencies should be concentrated at a small handful of high-performing “major emergency centres”.
GPs, local pharmacists, paramedics and the NHS 111 telephone triage service should all do more to keep people out of hospital, while A&E wards should be redefined, the report said. Under the plans, between 40 and 70 A&E units with the most specialist equipment and expertise will become the first port of call for around 5 per cent of patients with the most serious conditions – such as heart attacks and strokes – while another 70 to 100 will be known as “emergency centres” to treat serious conditions that may not require specialist intervention.
The report, which comes as the NHS braces itself for what doctors warn could be the “worst winter yet” for A&E overcrowding, sets out a three-to-five-year timeframe for reform. However, the Royal College of Emergency Medicine said the crisis was “here with us now” and warned that the NHS was failing to address drastic shortages in the number of doctors training for senior positions on casualty wards. One in five emergency admissions to hospital could have been avoided last year and 40 per cent of patients who attend A&E are discharged without treatment, the report said.
Its recommendations include GPs and social carers doing more to treat people in the community; 111 telephone services being enhanced to make it easier for patients to speak to clinicians; and paramedics receiving broader training and having better access to specialist advice in order to treat patients at the scene rather than bring them into hospital.
He said the reforms were “the only way to create a sustainable solution” to the crisis while maintaining “a rapid, high-quality and responsive service, free at the point of need”. He said: “The last time we had a systematic review of emergency care services was in the 1970s. Since then medical science has advanced dramatically, technology has advanced, society has changed. People are living longer, which brings multiple health problems, and expectations from the public have changed.”
He said that, in a rush to meet growing demand, the NHS had introduced more than 20 different “bolt-ons” to A&Es – such as walk-in centres, minor injury units and urgent care centres – which had created “a whole heap of confusion” about where patients should go to be treated. All such services should be grouped together under “a standardised name”, he said.
Plans for a two-tier A&E system – under the working title “emergency centres” and “major emergency centres” – are based on successful reforms to the way the NHS handles heart attack patients in a small number of specialist centres and the concentration of London’s stroke services from 32 to 8 hospitals – both of which have dramatically improved survival rates. The report was broadly welcomed by the medical profession, but the Royal College of Emergency Medicine said that problems on casualty wards were a result of a staffing crisis which the report did nothing to address.
“The current crisis is a lack of recruitment and subsequent retention of senior trainees and consultants in emergency medicine in the UK,” Dr Clifford Mann, the college’s president, said. “Any plan to provide emergency care must be based upon an adequate number of appropriately skilled clinicians and on this matter the review is disappointingly silent.”
Jeremy Hunt, the Health Secretary, said the NHS needed to change but that this would not happen “overnight”. “We’ve already taken action to help the NHS cope, investing £500m to help with winter pressures and agreeing a £3.8bn integration fund to look at joining up health and care services,” he said.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments